
Главная страница Случайная страница
Разделы сайта
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Methods of Examination 2 страница
|
|
Determining relative cardiac dullness. When determining the borders of relative cardiac dullness, interspaces should be percussed in order to avoid lateral distribution of vibrations along the ribs. The percussion stroke should be of medium strength. The pleximeter-finger should be tightly pressed against the chest so that the percussion vibration might penetrate deeper regions.
|
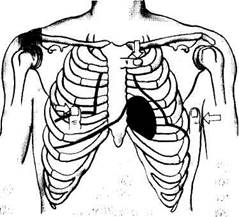
| Fig. 30. Position of the pleximeter-finger during outlining the upper, right, and left borders of relative cardiac dullness. |
When determining the border of relative dullness, the remotest points of the cardiac contour are first found on the right, then on the left, and finally at the top (Fig. 30). Since the border of cardiac dullness depends on the position of the diaphragm, the lower border of the right lung is first determined in the midclavicular line; its normal position is at the level of the 6th rib. The position of the lower border of the lung indicates the level
of the diaphragm. The pleximeter-finger is then moved one interspace above the lower border of the right lung and placed parallel to the right border of the heart being determined (normally, in the 4th costal interspace). Percussion is continued by moving the pleximeter-finger gradually along the interspace toward the heart until the percussion sound dulls. The right border of the heart is marked by the outer edge of the finger directed toward a clear resonant sound. Its normal position is 1 cm laterally of the right edge of the sternum.
The left border of the relative cardiac dullness is determined in the interspace, where the apex beat is present. The apex beat is therefore first determined by palpation, and the pleximeter-finger is then placed laterally of this point, parallel to the sought border, and the interspace is percussed toward the sternum. If the apex beat cannot be determined, the heart should be percussed in the 5th interspace from the anterior axillary line toward the sternum. The left border of relative cardiac dullness is located 1-2 cm medially of left midclavicular line; it coincides with the apex beat.
The upper border of the relative cardiac dullness is determined 1 cm to the left of the left sternal line. To that end, the pleximeter-finger is placed perpendicularly to the sternum, near its left margin, and then moved downward until dullness appears. The normal upper border of the relative cardiac dullness is in the 3rd interspace.
Once the area of relative cardiac dullness of the heart has been established, its transverse length is measured by a measuring tape, from the extreme points of the relative dullness to the anterior median line. The normal distance from the right border of relative cardiac dullness (usually in the 4th interspace) to the anterior median line is 3 or 4 cm, while the distance from the left border of relative cardiac dullness (usually in the 5th interspace) to the same line is 8 or 9 cm. The sum of these lengths is the transverse length of relative cardiac dullness (normally 11—13 cm).
The shape of the heart can be determined by percussion of the borders of the vascular bundle in the 2nd intercostal space on the right and left, and of relative cardiac dullness in the 4th or 3rd interspace on the right, and in the 5th, 4th, or 3rd interspace on the left. The pleximeter-finger is moved parallel to the borders of expected dullness and the elicited points of dullness are marked on the patient's skin. The points are then connected by a line to mark the contours of the relative cardiac dullness. Normally, an obtuse angle is formed by the lines of the left heart contour between the vascular bundle and the left ventricle. The heart is of normal configuration in such cases. In pathological conditions, when the chambers of the heart are dilated, mitral and aortal configurations are distinguished.
Determining absolute (superficial) cardiac dullness. The anterior wall of the heart is not covered by the lungs and the area of absolute cardiac
Special Part
dullness corresponds to the area of the heart. Percussion of this area gives dullness. To determine absolute dullness of the heart, light percussion strokes are needed. The right border of absolute cardiac dullness is first elicited. The pleximeter-finger is placed on the right border of relative (deep) cardiac dullness, parallel to the sternum, and then moved medially, to the left, to dullness. The border is marked by the outer edge of the finger directed toward resonance. In normal subjects this border passes along the left edge of the sternum.
To outline the left border of absolute cardiac dullness, the pleximeter-finger is placed slightly outside the border of relative cardiac dullness, and then moved medially to dullness. The left border of absolute cardiac dullness is normally 1-2 cm medially of the border of relative cardiac dullness. To elicit the upper border of absolute cardiac dullness, the pleximeter-finger is placed on the upper border of relative cardiac dullness and then moved downward to dullness. The superior border of absolute cardiac dullness is normally at the level of the 4th rib. It is sometimes difficult to differentiate between absolute and relative cardiac dullness, if percussion is done from the lungs to the heart. The pleximeter-finger should in such cases be placed at the centre of absolute dullness and then moved to its borders (from dullness to diminished dullness). The first sign of the admixed pulmonary resonance indicates the transition from the area of absolute dullness to the area of relative dullness.
The borders of the vascular bundle are determined by light percussion in the second intercostal space, to the right and left from the midclavicular line, toward the sternum. When the percussion sound dulls, a mark should be made by the outer edge of the finger. The right and left borders of vascular dullness are normally found along the edges of the sternum; the transverse length of dullness is 5—6 cm.
The area of cardiac dullness can be modified by extracardiac factors. At high position of the diaphragm, the heart assumes a horizontal position and its transverse dimensions thus increase. When the diaphragm is low, the heart assumes the vertical position and its transverse diameter is thus diminished. Accumulation of liquid or air in one pleural cavity displaces cardiac dullness toward the healthy side; in atelectasis and pneumosclerosis, or in the presence of pleuropericardial adhesion the borders of cardiac dullness are displaced to the affected side. The area of absolute cardiac dullness markedly diminishes or disappears in pulmonary emphysema, while it increases in pneumosclerosis. The area of absolute dullness is also enlarged in the anterior displacement of the heart (e.g. by a mediastinal tumour, due to accumulation of fluid in the pericardium, or in dilatation of the right ventricle). The borders of relative dullness are displaced in the presence of enlarged heart chambers. Displacement to the
right is due to dilatation of the right atrium and the right ventricle. If the left atrium or the conus of the pulmonary trunk is enlarged, the area of relative dullness is displaced upwards. Dilatation of the left ventricle displaces the area of relative dullness to the left. It should be remembered that a markedly enlarged and hypertrophied right ventricle displaces the left ventricle and can also displace the border of relative dullness to the left. Aortic dilatation increases the dullness area in the second interspace.
AUSCULTATION
Heart sounds. The sounds produced by a working heart are called heart sounds. Two sounds can be well heard in a healthy subject; the first sound, which is produced during systole and the second sound, which occurs during diastole.
In order to understand better the mechanism by which the heart sounds are produced, the phases of the cardiac cycle should be remembered. The heart contraction begins with the systole of the atria, which is followed by contraction of the ventricles. During the early systole the following phases are distinguished: (1) asynchronous contraction; the myocardium is involved only partly and the intraventricular pressure does not increase; (2) isometric contraction; it begins when the main mass of the myocardium is involved; atrioventricular valves are closed during this phase and the intraventricular pressure markedly increases; (3) ejection phase; the intraventricular pressure increases to level with that in the main vessels; the semilunar valves open. As soon as the blood has been ejected, the ventricles relax (diastole) and the semilunar valves close. The ventricles continue relaxing after the closure of the atrioventricular and semilunar valves until the pressure in them is lower than in the atria (isometric relaxation phase). The atrioventricular valves then open to admit blood into the ventricles. Since the difference between pressures in the atria and the ventricles is great during the early diastole, the ventricles are quickly filled (ventricle rapid filling phase). The blood flow then slows down (slow filling phase). Atrial systole begins, and the cardiac cycle is repeated.
The first sound is produced by several factors. One of them is the valve component, i.e. vibrations of the cusps of the atrioventricular valves during the isometric contraction phase, when the valves are closed. The second component is muscular, and is due to the myocardial isometric contraction. The intensity of myocardial and valvular vibrations depends on the rate of ventricular contractions: the higher the rate of their contractions and the faster the intraventricular pressure grows, the greater is the intensity of these vibrations. The first heart sound will thus be more resonant. The third component of the first heart sound is the vascular one. This is due to vibrations of the nearest portions of the aorta and the pulmonary trunk caused by their distention with the blood during the ejection phase. The fourth component is atrial; it is generated by vibrations caused by atrial contractions. This fourth component gives rise to the first sound since the atrial systole precedes the ventricular systole. Vibrations caused
Special Part
Chapter 6. Blood Circulatory System
by the atrial systole are normally blended with vibrations caused by the ventricular systole, and are heard as one sound.
The second sound is generated by vibrations arising at the early diastole when the semilunar cusps of the aortic valve and the pulmonary trunk are shut (the valve component) and by vibration of the walls at the point of origination of these vessels (the vascular component).
Both sounds can be heard over the entire precordium but their strength changes depending on the proximity of the valves involved in the formation of the first or second sound. Therefore, in order to assess correctly the findings of auscultation, it is necessary to know the sites where the valves project on the chest wall (the auscultatory valve areas) and also areas where the sounds produced by a valve can be better heard.
The sites of projections of the valves on the anterior chest wall are very close to one another (Fig. 31). The mitral valve projects to the left of the sternum, at the 3rd costosternal articutation, and the tricuspid valve, on the sternum midway between the 3rd left and 5th right costosternal articulations. The valve of the pulmonary trunk is projected in the 2nd intercostal space, to the left of the sternum; the aortic valve is projected in the middle of the sternum, at the level of the 3rd costosternal articulation. Since all heart valves are projected on a small area of the chest, it is difficult to decide which of them is damaged if the valves are auscultated at sites of their actual projections. Perception of sounds generated in the heart depends on the distance from the valve to its projection on the chest wall and on sound conduction by the course of the blood flow. It is

|
Fig. 31. Projection of the heart valves on the chest wall and listening points of the heart.
A —mitral valve; B —aortic valve; C —pulmonary trunk valve; D —tricuspid valve.
therefore possible to find certain sites on the chest where sounds of each valve can be better heard.
These auscultatory areas are as follows: (1) the area of the apex beat for the mitral valve because the vibrations are well transmitted by the firm muscle of the left ventricle and the cardiac apex is at the nearest distance to the anterior chest wall during systole; (2) the lower part of the sternum near its junction with the xiphoid process (the right-ventricular area); for the tricuspid valve; (3) the valve of the pulmonary trunk is best heard at its anatomical projection onto the chest, i.e. in the second intercostal space, to the left of the sternum; (4) the aortal valve is best heard in the second intercostal space, to the right of the sternum where the aorta is the nearest to the anterior chest wall. Moreover, the heart sounds which are associated with the contractions of the aortic valve or which develop during its affection, can be heard to the left of the sternum at the 3rd and 4th costosternal articulation (the so-called fifth listening post at the Botkin-Erb point).
Rules for auscultation of the heart. The heart is usually auscultated by a stethoscope or a phonendoscope, but direct (immediate) auscultation is also used. The condition of the patient permitting, the heart sounds should be heard in various postures of the patient: erect, recumbent, after exercise (e.g. after repeated squatting). Sounds associated with the mitral valve pathology are well heard when the patient lies on his left side, since the heart apex is at its nearest position to the chest wall; aortic valve defects are best heard when the patient is in the upright posture or when he lies on his right side. The heart sounds are better heard if the patient is asked to inhale deeply and then exhale deeply and keep breath for short periods of time so that the respiratory sounds should not interfere with auscultation of the heart. The valve sounds should be heard in the order of decreasing frequency of their affection. The mitral valve should be heard first (at the heart apex); next follows the aortic valve (in the second intercostal space to the right of the sternum), the pulmonary valve (in the second intercostal space, to the left of the sternum), tricuspid valve (at the base of the xiphoid process), and finally the aortic valve again at the Botkin-Erb point. If any deviations from normal sounds have been revealed at these points, the entire heart area should be auscultated thoroughly.
Normal heart sounds. The first sound is produced during systole, after a long pause. It is best heard at the heart apex since the systolic tension of the left ventricle is more pronounced than that of the right ventricle. The first sound is longer and louder than the second heart sound. The second sound is generated during diastole, after a short pause, and is best heard at the heart base because it is produced by the closure of the semilunar cusps of the aortic and pulmonary trunk valves. As distinct from the first sound, the second sound is shorter and higher. The tone of the heart sounds may
Special Part
Chapter 6. Blood Circulatory System
| Table 3 |
Differentition between the First and Second Heart Sounds
| First sound |
| Second sound |
 Main sign
Main sign
| Heart apex Follows the long pause 0.09-012 s Synchronous Synchronous |
| Heart base Follows the short pause 0.05-0.07 s Follows the apex beat Asynchronous |
 The best listening post Relation to cardiac pause
The best listening post Relation to cardiac pause
Duration Relation to apex beat
Relation to carotid pulse

 change in pathology, and in order to differentiate between the first and second sounds it should be remembered that the first sound coincides in time with the apex beat (if the latter can be palpated) or with the pulse of the aorta and the carotid artery. Table 3 gives signs that help differentiate between the first and second heart sounds.
change in pathology, and in order to differentiate between the first and second sounds it should be remembered that the first sound coincides in time with the apex beat (if the latter can be palpated) or with the pulse of the aorta and the carotid artery. Table 3 gives signs that help differentiate between the first and second heart sounds.
Sometimes the third and the fourth sounds can be heard, especially in children and in thin youths.
The third sound is caused by vibrations generated during quick passive filling of the ventricles with the blood from the atria during diastole of the heart; it arises in 0.15-1.12 s from the beginning of the second sound (Fig. 32).
The fourth sound is heard at the end of ventricular diastole and is produced by atrial contractions during quick filling of the ventricles with blood.
The third and fourth sounds are low-pitch and soft and are therefore hardly heard in normal subjects. But they are clearly seen on a phonocar-diogram. These sounds are better heard in immediate (direct) auscultation. The presence of the third and fourth sounds in the middle-aged usually indicates severe affection of the heart muscle.
Changes in the heart sounds. The heart sounds may increase or decrease their intensity, the tone, or length; they may be split or reduplicated, or adventitious sound may appear.
Intensity of the heart sounds may depend on conditions of the sound wave transmission, i.e. on the extracardiac causes. If subcutaneous fat or muscles of the chest are overdeveloped, or there are lung emphysema, liquid in the left pleural cavity, and some other affections that separate the heart from the anterior chest wall, the intensity of the heart sounds decreases. If conditions for sound transmission are improved (thin chest wall, the lung edges are sclerosed, the heart is pressed against the anterior chest wall by a growing tumour in the posterior mediastinum, etc.), the in-

Fig. 32. Formation of heart sounds.
a —atrial component (heard sometimes as an independent fourth sound); b —valvular component of the
first sound; c —muscular component of the first sound; d —vascular component of the first sound; e —
formation of the second sound; /—formation of the third sound.
tensity of the heart sounds increases. The sounds can also be increased by the resonance in large empty cavities filled with air (a large cavern in the lung, large gastric air-bubble). The intensity of the heart sounds also depends on the composition of the blood flowing through the heart: if the blood viscosity decreases (in anaemia) the intensity increases.
Variations in the heart sounds associated with affections of the heart proper are of great diagnostic importance.
The intensity of the heart sounds can decrease in decreased myocardial contractility in patients with myocarditis, myocardial dystrophy, car-diosclerosis, collapse, and accumulation of fluid in the pericardial cavity.
Both heart sounds can be increased due to the effect of the sympathetic nervous, system on the heart. It occurs in physical and emotional strain, during exercise, and in patients with exophthalmic goitre.
Changes in only one heart sound is very important diagnostically.
Special Part
Chapter 6. Blood Circulatory System
The intensity of the first heart sound diminishes in the mitral and aortic valve insufficiency. The cusps of the affected mitral valve fail to close completely the left atrioventricular orifice during systole. Part of the blood is thus regurgitated to the left atrium. The pressure of the blood against the ventricular walls and the cusps of the mitral valve is below normal, and the valvular and muscular components of the first heart sound markedly diminish. The period of closed valves is absent also during systole in the aortic valve insufficiency. It means that the valvular and muscle components of the first heart sound will also diminish significantly.
In tricuspid and pulmonary valve failure, the diminution of the first heart sound will be better heard at the base of the xiphoid process due to the diminution of the muscular and valvular components of the right ventricle.
The first sound can be diminished at the heart apex in stenotic aortal orifice because systolic tension of the myocardium grows slowly when the blood flow from the left ventricle is obstructed and it is overfilled with blood; the amplitude of the sound vibrations decreases. In diffuse affections of the myocardium (due to dystrophy, cardiosclerosis or myocarditis), the first heart sound only may be diminished because its muscular component also diminishes in these cases.
The first sound increases at the heart apex if the left ventricle is not adequately filled with blood during diastole. The first sound often becomes louder in stenosis of the left atrioventricular orifice, when less than normal amount of blood is discharged from atrium to the ventricle during diastole. The muscle of the left ventricle is therefore less distended by the blood by the start of systole; it is more relaxed and therefore contracts more rapidly and energetically to intensify the first sound. The first sound increases in stenosed right atrioventricular orifice at the base of the xiphoid process. This sound is also intensified during extrasystole (premature contraction of the heart) due to inadequate diastolic filling of the ventricles.
The variation of the first sound at the heart base is not important because this sound is transmitted here from its best auscultative area, i.e. from the cardiac apex area. The second heart sound is heard over the base. In normal cases the intensity of this sound over the aorta is the same as over the pulmonary trunk. Although the blood pressure in the aorta is higher and the cusps of its valve are closed with a greater force than those' of the pulmonary valve, the sound produced by the closing aortic valve is perceived by the examiner as being of the same intensity as the sound of the pulmonary valve, because of the deeper location of the aortic valve.
The second sound over the aorta is diminished in aortic valve affections because either the cusps of the valve are destroyed or their vibrating power decreases due to developing cicatrices. Moreover, the thrust of the blood
discharged at early diastole from the aorta to the cusps of the aortic valve is weaker than in normal persons because part of the blood is regurgitated to the ventricle through an incompletely closed aortic orifice. The second sound can be inaudible over the aorta if the aortic valve is much destroyed. The second sound diminishes over the aorta in cases with marked hypotension; the second sound diminishes over the pulmonary trunk in cases with aortic valve incompetence (in very rare cases) and in decreased pressure in the lesser circulation.
The second sound may increase either over the aorta or over the pulmonary trunk. If the sound is more intense over the aorta, it is said to be accentuated over the aorta, and if it is stronger over the pulmonary trunk, accentuation of the second sound over pulmonary artery is meant.
The aortic second sound is accentuated when the blood pressure in aorta increases (in essential hypertension, during heavy exercise, in psychic excitation), because during early diastole, the aortic valve cusps are closed with a greater force due to increased blood pressure in the aorta. The tone of the second heart sound over the aorta often varies. For example, in patients with sclerotic aortic valve, the second sound over the aorta acquires a metallic character which, however, can be heard in normal arterial pressure as well.
The accentuated second sound over the pulmonary artery occurs when pressure in the lesser circulation is elevated or when the vessels of the lesser circulation are overfilled with blood (e.g. in mitral heart diseases), deranged circulation in the lungs and stenosed pulmonary artery (in lung emphysema or pneumosclerosis).
Reduplication of the heart sounds may be revealed by auscultation. Two short sounds which quickly follow one another are heard instead of one. Reduplication of the sounds occurs in asynchronous work of the left and right chambers of the heart. Asynchronous closure of the atrioventricular valves splits the first sound while asynchronous closure of the semilunar valves causes reduplication of the second heart sound. If the two short sounds follow one another at a short interval, they are not perceived as two separate sounds, the sound is said to be split. Both physiological and pathological splitting of the heart sounds are possible. Physiological reduplication or splitting of the first sound is due to asynchronous closure of the atrioventricular valves, e.g. during very deep expiration, when the blood is ejected into the left atrium with a greater force to prevent the closure of the mitral valve; the valvular component of the left ventricle is therefore split and is perceived as a separate sound.
Pathological reduplication of the first sound can occur in impaired in-traventricular conduction (through the His bundle) as a result of delayed systole of one of the ventricles.
Special Part
Chapter 6. Blood Circulatory System

|
The second sound is reduplicated more frequently than the first heart sound. Reduplication occurs due to asynchronous closure of the valve of the aorta and pulmonary trunk because of the different length of contractions of the left and the right ventricles. The length of the ventricular systole depends on the volume of the ejected blood and the pressure in that vessel (aorta or the pulmonary artery) into which the blood is expelled. When the amount of blood in the left ventricle decreases and the pressure in the aorta is low, systole of the left ventricle ends sooner and the aortic valve cusps will close earlier than the cusps of the valve of the pulmonary trunk. The second heart sound can therefore be duplicated in cases with diminished or increased filling of one of the ventricles or when pressure in the aorta or the pulmonary artery changes. Physiological reduplication of the second sound is mostly connected with various respiratory phases: the filling of the right and left ventricles differs during inspiration and expiration and the length of their systole changes accordingly, as well as the time of closure of the valve of the aorta and pulmonary trunk. The amount of blood flowing to the left ventricle decreases during inspiration because part of blood is retained in the distended vessels of the lungs. The left-ventricular systolic blood volume decreases during inspiration, its systole ends earlier, and the aortic valve therefore closes earlier as well. At the same time, the stroke volume of the right ventricle increases, its systole prolongs, the pulmonary valve closure is delayed and the second sound is thus doubled.
Pathological reduplication of the second sound can be due to delayed closure of the aortic valve in persons suffering from essential hypertension, or if the closure of the pulmonary valve is delayed at increased pressure in the lesser circulation (e.g. in mitral stenosis or emphysema of the lungs), delayed contraction of one of the ventricles in patients with bundle-branch block.
True reduplication of the heart sounds should be differentiated from apparent doubling which is connected with the appearance of adventitious sounds. The mitral valve opening sound is an example. This sound is heard at the heart apex of patients with mitral stenosis. The sound is heard 0.07-0.13 s following the second sound, during diastole. In normal conditions, the cusps of the atrioventricular valve open noiselessly, they are freely forced back by the blood flow ejected from the atria to the ventricles. In mitral stenosis, the cusps of the sclerosed valve adhere to each other by their edges and cannot freely move to the walls of the ventricle. Therefore, blood thrusts against the valve as it passes from the atrium to generate sound vibrations that are responsible for the appearance of adventitious sounds.
|
|