
Главная страница Случайная страница
Разделы сайта
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Methods of Examination 2 страница. In accumulation of much fluid in the abdominal cavity, ballotment should be used to palpate the liver
|
|
In accumulation of much fluid in the abdominal cavity, ballotment should be used to palpate the liver. To that end the right hand (two or four flexed fingers) should be placed on the lower right part of the abdomen, perpendicularly to the expected lower edge of the liver. The abdominal wall is given a sharp tap from the palpating fingers which move upward to meet the firm object, the liver, which is first tossed to the deeper parts of the abdominal cavity but is then returned back to strike the fingers.
Palpation is painful if the liver is inflamed and the affection extends onto the liver capsule; the liver is also tender when it is distended (e.g. in blood congestion due to heart failure). The liver of a healthy subject (if it is accessible to palpation) is soft; it becomes firmer in hepatitis, hepatosis, and cardiac congestion. The liver is especially firm in cirrhosis. Its edge becomes sharp and the surface smooth or covered with small tubercles. The liver is also firm in the presence of tumour and multiple metastases of cancer. Its surface then becomes covered with rough tubercles (surface metastases) and the lower margin is rough. The liver is firm in amyloidosis. Comparatively small tumours and echinococcosis can sometimes be palpated. Protrusion of the lower margin of an enlarged liver is assessed with respect to the costal arch in the right anterior axillary line, right midclavicular line, right parasternal line, anterior median line, and left parasternal line. Palpation verifies the findings obtained by percussion of the liver.
The gall bladder cannot be palpated in healthy subjects because of its soft consistency and the insignificant protrusion. But if the gall bladder is enlarged (hydrops, stones in the bladder, cancer, etc.) it becomes palpable. The position of the patient for palpation of the gall bladder is the same as in palpation of the liver. After the margin of the liver has been found, the gall bladder should be palpated at the lateral edge of the right rectus ab-dominis muscle. The palpation technique is the same as that for palpation of the liver. The gall bladder can easier be found by moving the palpating fingers in the direction perpendicular to the axis of the gall bladder. The bladder is felt like a pear of variable size, firmness and tenderness depending on the character of pathology in the gall bladder proper or the sur-
if;
Special Part
Rounding organs (e.g. the gall bladder is enlarged, soft, and elastic in tumour-obstructed bile duct: Courvoisier-Terrier sign; the bladder is firm and tuberous in the presence of newgrowths in its wall, in overfilling with stones, in inflammation of the wall, etc.). An enlarged gall bladder is mobile during respiration (it performs lateral pendulum-like movements). The gall bladder loses its mobility in inflammation of the overlying peritoneum (pericholecystitis). In the presence of cholecystitis and cholelithiasis, the palpation is difficult because of sharp pain and reflectory rigidity of the muscles of the anterior abdominal wall.
The described technique of palpation of the liver and the gall bladder is simple and effective. Difficulties encountered in palpation and also the belief that only palpation can give valuable diagnostic information have stimulated the search for new palpation techniques. But most of them differ only in the position of the examining hands (Glenard, Mathieu, Chaufard, Chiray) or the position of the physician himself with respect to the patient during examination. For example, the liver and the gall bladder are examined (according to Chiray) from behind the leaning patient; the liver edge is palpated by two hands simultaneously, one hand feeling the liver from below and the other from top (according to Gilbert). But none of these techniques used for palpation of the liver and the gall bladder can boast of having significant advantages over others. Success of palpation depends not on the variety of techniques but on the experience of the examiner.
AUSCULTATION
The importance of auscultation for diagnosis of diseases of the liver and gall bladder is only relative. In only rare cases peritoneal friction can be heard over the liver and the gall bladder (in perihepatitis or pericholecystitis). This sound resembles pleural friction, and is a dangerous sign. It indicates deep extension of inflammation onto all walls of the gall bladder and possible perforation.
Chapter 7. Digestive System
Most functional tests impose increased loads on the studied organ. The load is usually so high that an affected organ cannot meet the new conditions. Functional tests for liver are intended to reveal the specific activity of this organ, e.g. detoxicating or protein and pigment forming function. These tests demonstrate only partially the liver function, because the liver is not involved independently in some types of metabolism, but is connected with the other organs in their complex involvement. Tests for carbohydrate, water, and fat metabolism are examples of such tests.
Pigmentary metabolism. Concentration of bilirubin and its reduction products in the blood, faeces, and urine demonstrate the pigment function of the liver. Deranged pigment metabolism indicates disordered functional condition of hepatocytes and helps differentiate between various types of jaundice.
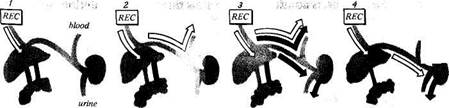
Bilirubin is formed in the reticulo-endothelial cells of the bone marrow, lymph nodes, and mainly in the spleen and the stellar reticuloendotheliocytes of the liver (Fig. 94). Bilirubin is formed from haemoglobin which is released during the physiological break-down of erythrocytes. Haemoglobin breaks down into the globin and haem (containing iron). Unbound bilirubin is formed in the cells of the reticulohistiocytary system from the released haem. Bilirubin circulates in the blood, being loosely connected with protein. The normal blood bilirubin content is 8.55-20.52 mmol/1 (from 0.5 to 1.2 mg/100 ml). The main bulk of unbound bilirubin is supplied to the liver where it is disjoined from albumin and bound (by the agency of the liver enzymes) by glucuronic acid to form water-soluble bilirubin glucuronide (mono- and diglucuronide or " bound biliburin") which is released into the bile ducts.
The liver thus participates in bilirubin metabolism to perform the following functions: (1) formation of bilirubin in stellar reticulo-endothelial cells; (2) capture of unbound bilirubin from blood; (3) formation of bilirubin compounds with glucuronic acid; (4) secretion of bilirubin glucuronide (bound bilirubin) into bile.
 | |||||
 |  | ||||
| t |
 Laboratory and Instrumental Methods
Laboratory and Instrumental Methods
FUNCTIONAL STUDY OF THE LIVER
Not all functions are affected in an involved liver; the dysfunctions are not simultaneous, and their degree is different. The reserves of the liver are significant: preservation of 20 per cent of the functioning parenchyma is sufficient to maintain vital activity of experimental animals. The regenerative power of the liver is great too. Therefore, certain hypofunction of the liver cannot bear substantial effect on the patient's condition: the affected liver is able to maintain the main vital processes in the new conditions.
faeces
unbound bilirubin bound bilirubin
Fig. 94. Secretion of bilirubin in norm (/), in haemolytic jaundice (2); in parenchymatous jaundice (3), and in obstructive jaundice (4).,
Special Part
Chapter 7. Digestive System
 Early in the 20th century, van den Bergh noted different reaction of jaundice serum with sulphodiazo reagent in jaundice of various aetiology. The serum of a patient with obstructive jaundice turned red immediately after the diazo reagent was added, while the serum of a patient with haemolytic jaundice turned red only after alcohol was added. The first reaction was called " direct" and the second " indirect". Unbound bilirubin gives indirect reaction while bilirubin glucuronide gives a direct reaction. Depending on the number of molecules (one or two) of glucuronic acid added to the bilirubin molecule, mono- or diglucuronide of bilirubin is formed.
Early in the 20th century, van den Bergh noted different reaction of jaundice serum with sulphodiazo reagent in jaundice of various aetiology. The serum of a patient with obstructive jaundice turned red immediately after the diazo reagent was added, while the serum of a patient with haemolytic jaundice turned red only after alcohol was added. The first reaction was called " direct" and the second " indirect". Unbound bilirubin gives indirect reaction while bilirubin glucuronide gives a direct reaction. Depending on the number of molecules (one or two) of glucuronic acid added to the bilirubin molecule, mono- or diglucuronide of bilirubin is formed.
The blood of healthy people contains only free liver pigment. In diseases attended by disordered or perverted bound-bilirubin excretion with bile, the bound bilirubin enters blood and both pigments then become involved in the circulation. (They can be determined separalety.) Van der Bergh's qualitative test gives only tentative information: if the reaction is indirect, it may be considered that unbound bilirubin alone is present in the blood; if the reaction is direct, the proportion of both pigments in the blood is unknown because the positive direct reaction masks the presence of any quantity of unbound bilirubin. The bilirubin fractions are now determined separately. The same diazo reagents (as in qualitative tests) are used in most techniques. Diazo reagent I is prepared by dissolving 5 g of sulphanylic acid and 15 ml of strong hydrochloric acid in distilled water, which is then added to make 1 litre. Diazo reagent II is a 0.5 per cent solution of sodium nitrite. (The diazo mixture consists of 10 ml of solution I and 0.25 ml of solution II.)
Qualitative test: 0.25 ml of the diazo mixture is added to 0.5 ml of serum. If the mixture turns red sooner than in 1 min, the reaction is quick direct to indicate the presence of bound bilirubin in the serum. If the colour changes slowly (within 1—10 min), the bound bilirubin content is relatively small; the reaction is considered to be slow direct. If the solution turns red in more than ten minutes, the direct reaction is considered to be negative. If it is necessary to make sure that the yellow colour of the serum depends on the presence of bilirubin, a double quantity of alcohol is added, the solution is passed through a filter, and the diazo mixture is added to the filtrate: pink colour develops (indirect reaction).
There are many methods for quantitative determination of the bilirubin fractions. Some of them are based on the reaction of bilirubin with the diazo reagent in the presence of caffeine (which is used in a common Jen-drassik test), methyl alcohol, and some other reagents which act like a catalyst. The total amount of both fractions contained in the serum treated with the catalyst can be determined. Only bound pigment is determined in
another portion of the serum containing no catalyst. The amount of free bilirubin can be found by subtracting the bound fraction from the total bilirubin content of the blood. Other methods for separate determination of bilirubin fractions (chemical, chromatographic) are more complicated.
Unbound bilirubin is insoluble in water and cannot be excreted by the kidneys. When bound with glucuronic acid it becomes soluble and can be determined in the urine of patients with subhepatic and hepatic jaundice. Only bound bilirubin (bilirubin glucuronide) is excreted into the bile ducts. A small portion of bilirubin is reduced to urobilinogen in the large bile ducts and the gall bladder (especially if they are affected by inflammation) and farther in the intestine. Urobilinogen is resorbed in the upper portion of the small intestine and delivered to the liver with the blood of the portal vein. A healthy liver completely traps it and oxidizes, but an affected liver cannot perform this function and urobilinogen passes into blood and is excreted with urine as urobilin. Urobilinuria is an early and very sensitive sign of liver dysfunction. The greater portion of bilirubin is reduced in the intestine to stercobilinogen. Its main portion is excreted with faeces in which it is converted into stercobilin to give faeces its normal colour (upon exposure to air and light). A small portion of stercobilinogen is absorbed in the lower portions of the large intestine, bypasses the liver, and enters the general circulation through the haemorrhoidal veins to be excreted by the kidneys. Normal urine always contains traces of stercobilinogen which converts into stercobilin on exposure to air and light.
Most reactions by which products of bilirubin reduction are discovered in urine give similar results with both urobilin and stercobilin, although these two compounds differ in their chemical structure and physical properties. Methods of their separation are relatively complicated. They are therefore determined together and designated by a common name of urobilinoids.
Urobilin content of the urine increases not only in the presence of hepatic insufficiency, but also in increased haemolysis. In this case, due to release of considerable quantity of haemoglobin, greater amounts of bilirubin are produced and liberated into the intestine. Increased production of stercobilin intensifies its excretion with urine. In obstructive jaundice, when bile is not supplied to the intestine, stercobilin is absent from faeces and the urine is free from urobilin casts. Bilirubin excretion with bile and stercobilin content of faeces decrease in hepatic jaundice, while urobilin casts of urine increase. Their normal ratio is from 10: 1 to 20: 1, but in pathology it decreases significantly, and is as low as 1: 1 in severe liver affections.
Stercobilin content of faeces in haemolytic jaundice exceeds significantly urobilin excretion in the urine. Their ratio increases to 300: 1-500: 1.
Special Part
The ratio between the bilirubin reduction products in faeces and urine is much more informative for differentiation of various types of jaundice than the absolute content of each substance.
Carbohydrate metabolism. With participation of the enzyme systems, liver cells synthesize glycogen and deposit it; glycogenolysis and glyconeogenesis also occur here. The normal sugar content of blood is maintained also by some other organs and systems, such as the pancreas, the pituitary-adrenal system, etc. In this connection, the blood sugar content with the fasting stomach changes only in very severe liver affections, and therefore functional tests can only reveal carbohydrate hypofunction of the liver. The glucose tolerance test is not effective because the blood glucose content depends not only on the above-mentioned organs but also on the condition of the vegetative nervous system, on the glycogen stores in the liver and muscles, and some other factors.
The galactose tolerance test is an effective method to assess the liver function. Galactose is not assimilated by the bodily tissues or organs except the liver; its blood content does not depend on hormones. The patient is given to drink a solution of 40 g of galactose in 200 ml of water, and galactose excretion in the urine is then determined. Normally maximum 3 g of galactose are excreted in 4 hours. The renal function and the absorption power of the intestine may affect galactose excretion in the urine, and the determination of galactose in the blood is therefore more reliable. The maximum rise of the blood sugar occurs in 30-60 minutes with the normal liver function. The maximum level does not exceed 150 per cent of the initial one, which is restored in two hours. If the liver function is inadequate, the sugar level is higher, while the decrease in the galactose level in the blood is slower.
The glycogenolysis function is determined by the adrenaline test. The patient is given subcutaneously 1 ml of a 0.1 per cent adrenaline solution. In healthy subjects this injection increases the blood sugar level by at least 50 per cent. If the liver is affected, no rise is observed.
The role of the liver in the protein metabolism is very important: the liver synthesizes and retains proteins. Amino acids, polypeptides of food, and products of breakdown of tissue proteins are delivered into the liver with blood where they are catabolized, detoxicated, and the unused breakdown products are removed. Some amino acids are deaminated and reaminated. The released ammonia is converted by the liver into less toxic urea. Amino acids (both produced by the liver and carried from outside) are used by the liver to build proteins of its own tissue and also blood proteins: albumin, globulins, (alpha, beta, and to a certain extent gamma globulins), fibrinogen, prothrombin, heparin, and certain enzymes. The liver synthesizes also compounds of proteins with lipids (lipoproteins) and
I
Chapter 7. Digestive System
carbohydrates (glycoproteins). The disorder in the protein-synthesizing function of the liver is revealed by studying the proteins of the blood plasma or serum. This dysfunction has its effect not only on the total protein content but also on the ratio of its different fractions, which is more important diagnostically: the upset protein ratio (dysproteinaemia) is characteristic of most liver pathologies.
Paper electrophoresis is widely used in clinic now. Depending on the size and shape of molecules, their charge, and some other factors, various proteins move at different velocities toward the positive electrode. Various protein fractions concentrate on different portions of paper during electrophoresis; proteins are then revealed by staining. The content of each separate fraction is determined by colour intensity. Proteins of the blood plasma are separated into five main fractions: albumins, alpha^ alpha2, beta, and also gamma globulins (see Table 4). Electrophoresis in other media (agar, starch gel, etc.) separates proteins into greater quantity of fractions.
Table 4
| Fraction |
Normal Proteinogram
| average |
 Normal percentage
Normal percentage
 variation
variation
| 56.3-68.8 32.0-43.0 3.0- 5.8 6.9-10.5 7.3-12.5 12.8-19.2 |
| 60.9 39.1 4.2 8.2 11.5 15.2 1.2-2 |
Albumins Globulins:
alpha j
alpha2
beta
gamma A-G ratio
 The A-G ratio most frequently decreases in liver diseases. This occurs mainly due to the decrease in the albumin content (their upset synthesis). In patients with acute inflammation of the liver (acute hepatitis) the content of alpha2 globulins in the blood plasma increases, while in chronic hepatitis the gamma globulin content increases probably due to accumulation of antibodies which move during electrophoresis with gamma globulins. The total serum protein content often increases as well. The total protein content decreases sharply (at the expense of albumins) in patients with liver cirrhosis; the content of gamma globulins, however, increases markedly.
The A-G ratio most frequently decreases in liver diseases. This occurs mainly due to the decrease in the albumin content (their upset synthesis). In patients with acute inflammation of the liver (acute hepatitis) the content of alpha2 globulins in the blood plasma increases, while in chronic hepatitis the gamma globulin content increases probably due to accumulation of antibodies which move during electrophoresis with gamma globulins. The total serum protein content often increases as well. The total protein content decreases sharply (at the expense of albumins) in patients with liver cirrhosis; the content of gamma globulins, however, increases markedly.
During electrophoresis, fibrinogen migrates together with gamma globulins and cannot be detected separately. For quantitative determination of fibrinogen, it is precipitated from plasma by calcium chloride with
Special Part
Chapter 7. Digestive System
 subsequent weighing of the washed and dried precipitate, or by determining protein in the precipitate after its dissolution. Fibrinogen is synthesized in the liver and its content of plasma therefore decreases significantly if the liver is seriously affected. This affects blood coagulation. The normal fibrinogen content of plasma is from 200 to 400 mg/100 ml (2-4 g/1 or 8—13 mg/ml; clot weight).
subsequent weighing of the washed and dried precipitate, or by determining protein in the precipitate after its dissolution. Fibrinogen is synthesized in the liver and its content of plasma therefore decreases significantly if the liver is seriously affected. This affects blood coagulation. The normal fibrinogen content of plasma is from 200 to 400 mg/100 ml (2-4 g/1 or 8—13 mg/ml; clot weight).
The total plasma protein content is determined mostly by the refrac-tometric method; if a refractometer is not available, chemical methods can be used (Kjeldahl method, biuret test, nephelometric method, etc.).
The ratio of the protein fractions can also be determined by im-munoelectrophoresis, ultracentrifuging, etc. In addition to direct determination of the ratio of the protein fractions, dysproteinaemia can also be determined by simple methods. These are the so-called protein sedimentation (flocculation) tests. In the presence of dysproteinaemia (especially in decreased albumin content) the equilibrium of the colloidal blood system becomes upset. This disturbance can be revealed by adding electrolyte to the blood serum in the concentration that would not alter normal serum but in dysproteinaemia would cause cloudiness or precipitation of flakes (protein flocculation). The presence of paraproteins (pathological proteins) can also be detected in the blood. These tests include reactions with corrosive sublimate (Takata-Ara test, Grinsted and Gross sublimate tests), zinc sulphate, cadmium sulphate, Lugol's iodine solutions, etc. In another group of flocculation tests the stability of a colloidal solution is upset by adding a small portion of dys- or paraproteinaemic serum (thymol, colloidal gold test, etc.).
The thymol turbidity test is based on determination of turbidity of a colloidal thymol reagent caused by adding 1/60 volume of serum. The test is positive mostly in the increased blood serum beta-lipoprotein content. It is always positive in virus hepatitis and diffuse affections of the liver. It is negative in obstructive jaundice.
In the presence of significant excess of globulins, and especially of fibrinogen, the formol-gel test becomes positive (the serum converts into a gel from the addition of formaldehyde).
Dozens of sedimentation tests have been proposed. They all are nonspecific and are positive not only in the presence of liver diseases but also in multiple myeloma, collagenosis, etc. These tests reveal dysproteinaemia more easily than electrophoresis.
Prothrombin (factor II of blood coagulation) is synthesized in the liver with participation of vitamin K. The cause of hypoprothrombinaemia is either upset synthesis of prothrombin by the hepatocytes or vitamin K deficiency (vitamin K is fat-soluble and is delivered to the liver from the intestine). In the presence of obstructive jaundice, when absorption of fats
and vitamin K is deranged due to the obstructed delivery of bile acid to the intestine, the synthesis of prothrombin in the liver decreases and the blood prothrombin content decreases as well. In order to reveal the cause of hypoprothrombinaemia, a test with parenteral administration of vitamin K is used. If the blood prothrombin content increases after administration of vitamin K, the prothrombin synthesizing function of the liver is normal. This test helps differentiate between obstructive and parenchymatous jaundice. Prothrombin is determined by the rate of coagulation of recalcified plasma in the presence of excess thromboplastin.
Amino acids, urea, residual nitrogen and ammonia are the products of protein decomposition which have a certain diagnostic importance. The total blood content of amino acids increases only in severe affections of the liver with impairment of its deaminating and urea-forming functions (otherwise rather stable). The condition for the increase in residual nitrogen of blood is a simultaneous renal dysfunction. Increased residual nitrogen occurring in renal insufficiency alone differs from that occurring in hepatorenal insufficiency by the main component of residual nitrogen. This is urea in renal insufficiency and amino acids in hepatorenal dysfunction. Separate determination of amino acids of the blood by chromatographic methods does not give reliable diagnostic information and the labour-consuming chromatographic procedure is not thus justified. Determination of leucine and tyrosine crystals that appear in the urine sediment in the presence of acute dystrophy of the liver is of certain diagnostic importance.
The blood ammonia content increases when the liver is unable to detox-icate ammonia delivered from the intestine (by synthesizing urea). Accumulation of ammonia in the blood produces a toxic effect on the central nervous system. Hyperammoniaemia is therefore a forerunner of hepatic coma.
The importance of the liver is especially great in fat metabolism. The liver performs the decisive role in the synthesis and splitting of fats, phospholipids, and cholesterol, in esterification and liberation of cholesterol, and in maintaining constant cholesterol content of blood. Blood lipids change their concentration in liver affections. Normal blood serum cholesterol content is 3.9-5.2 mmole/1 (150-200 mg/100 ml). The cholesterol concentration decreases in patients with severe forms of acute and chronic hepatitis and cirrhosis of the liver. Cholesterol increases in most obstructive jaundices. The activity of alkaline phosphatase usually increases simultaneously. But these quantitative shifts are not always demonstrative. The degree of esterification of cholesterol (their combination with fatty acids), which occurs mostly in the liver, is more informative diagnostically. Normally 60-70 per cent of blood cholesterol is ester-
Special Part
Chapter 7. Digestive System
 bound, but this percentage decreases in liver affections due to the decreased esterase activity. The decrease is proportional to the degree of liver dysfunction. The ratio of the ester-bound cholesterol to the total blood cholesterol (normally 0.6-0.7) is called esterification coefficient. When markedly decreased, this coefficient is a poor prognostic sign.
bound, but this percentage decreases in liver affections due to the decreased esterase activity. The decrease is proportional to the degree of liver dysfunction. The ratio of the ester-bound cholesterol to the total blood cholesterol (normally 0.6-0.7) is called esterification coefficient. When markedly decreased, this coefficient is a poor prognostic sign.
The blood phospholipid content in the presence of liver pathology changes mainly in the same way as the content of cholesterol. The blood content of lipoprotein fractions is also affected by liver diseases.
Certain blood microelements are important diagnostically. The most informative are iron and copper. Both elements are contained in the serum as metal proteids, i.e. compounds with proteins, in which they are present in microgram quantities. These metals are also present in the liver, which serves as a depot for them. Iron is deposited in the liver as ferritin, an iron-protein complex, that is a reserve of iron used for the synthesis of haemoglobin in the bone marrow. Another iron compound is haemosiderin, the product of haemoglobin decomposition, which is accumulated in the liver in increased haemolysis and also in some diseases. Transferrin (the transport protein) which carries iron from the liver to the bone marrow is also synthesized in the liver. Iron that is not bound in haemoglobin is also determined in the blood serum for diagnostic purposes: its content increases significantly (2—3 times) in acute hepatitis; in chronic hepatitis and cirrhosis the increase is less significant, while it does not change (or even decreases) in obstructive jaundice.
Copper is contained in the blood as an oxidative enzyme ceruloplasmin; it is also contained in the liver as a copper-containing protein hepatocuprein. The blood serum copper content slightly increases in hepatitis, and the increase is pronounced in obstructive jaundice. The iron to copper ratio is always decreased in obstructive jaundice and is mostly increased in parenchymatous affections of the liver.
Study of liver enzymes. The liver cells contain numerous enzymes regulating metabolic processes in the liver. Affection of hepatocytes causes an increased excretion into the blood of some enzymes, while the synthesis of other enzymes decreases. Changes in activity of enzymes in the blood serum, which are a sensitive and quick response to liver affections, are widely used for diagnostic purposes. Some of these enzymes are produced not only by the liver but also by some other organs. But changes occurring in some enzymes during liver pathology are so constant that their determination becomes of great practical value. These are transaminase, aldolase, alkaline phosphatase, cholinesterase, lactic dehydrogenase (see Table 12).
Determination of isoenzymes of certain enzymes mentioned above gives more reliable diagnostic information. Isoenzymes are group of enzymes
that have similar catalytic action but differ in the structure of their proteins. During electrophoresis in starch gel, an isolated enzyme is subdivided into isoenzymes due to their different electrophoretic mobility.
|
|