
Главная страница Случайная страница
Разделы сайта
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Methods of Examination
|
|
Inquiry
Complaints. Patients with diseases of the stomach complain of poor appetite, perverted taste, regurgitation, heartburn, nausea, vomiting, epigastric pain, and haematemesis. Regurgitation, heartburn, nausea, vomiting, and the feeling of overfilled stomach after meals are the group of the so-called dyspeptic complaints. These symptoms may be observed in diseases of some other organs and systems. Determining the specific character of each symptom is important during inquiry of the patient.
Deranged (poor or increased) appetite occurs in infectious diseases, metabolic disorders, etc. Poor appetite or its complete absence (anorexia) is usually characteristic of gastric cancer. This symptom is often an early sign of cancer. Appetite often increases in peptic ulcer, especially in duodenal ulcer. Loss of appetite should be differentiated from cases when the patient abstains from food for fear of pain (cibophobia). This condition often occurs in subjects with gastric ulcer, though their appetite is increased.
Perverted appetite that sometimes occurs in patients is characterized by the desire to eat inedible materials such as charcoal, chalk, kerosine, etc.
23-1556
Special Part
Chapter 7. Digestive System


 Appetite is perverted in pregnant women and in persons suffering from achlorhydria. Some patients with cancer of the stomach or some other organs often feel aversion to meat. The developmental mechanism of appetite is connected with excitation of the food centre (according to Pavlov). Excitation or inhibition of this centre depends on impulses arriving from the cerebral cortex, on the condition of the vegetative centres (excitation of the vomiting centre causes loss of appetite), and on reflex effects from the alimentary organs. The multitude of factors that act on the food centre account for the high variation in appetite.
Appetite is perverted in pregnant women and in persons suffering from achlorhydria. Some patients with cancer of the stomach or some other organs often feel aversion to meat. The developmental mechanism of appetite is connected with excitation of the food centre (according to Pavlov). Excitation or inhibition of this centre depends on impulses arriving from the cerebral cortex, on the condition of the vegetative centres (excitation of the vomiting centre causes loss of appetite), and on reflex effects from the alimentary organs. The multitude of factors that act on the food centre account for the high variation in appetite.
Taste may be perverted due to the presence of unpleasant taste in the mouth and partial loss of taste in an individual. It can often be associated with some pathology in the mouth, e.g. caries or chronic tonsillitis. A coated tongue can be another cause of unpleasant taste in the mouth.
Regurgitation usually implies two phenomena: a sudden and sometimes loud uprise of wind from the stomach or oesophagus (eructation), and the return of swallowed food into the mouth (sometimes together with air). Regurgitation depends on contraction of the oesophageal muscles with the open cardia. Regurgitation may be due to air swallowing (aerophagy). It is heard at a distance and occurs in psychoneurosis. In the presence of motor dysfunction of the stomach, fermentation and putrefaction of food with increased formation of gas occur in the stomach (the phenomenon otherwise absent in norm). In abnormal fermentation in the stomach, the eructated air is either odourless or smells of bitter oil, which is due to the presence of butyric, lactic and other organic acids that are produced during fermentation in the stomach. In the presence of abnormal putrefaction, the belched air has the odour of rotten eggs (hydrogen sulphide). Bitter belching indicates intensive degradation of proteins. Belching is characteristic of stenosed pylorus with great distention of the stomach and significant congestion in it. Acid regurgitation is usually associated with hypersecretion of gastric juice and occurs mostly during pain attacks in ulcer. But it can also occur in normal or insufficient secretion of the stomach in the presence of insufficiency of the cardia (when the stomach contents are regurgitated into the oesophagus). Bitter regurgitation occurs ' in cases with belching up of bile into the stomach from the duodenum, and also in hyperchlorhydria; bitterness depends on the bitter taste of peptones.
Pyrosis is otherwise known as heartburn, i.e. burning pain in the epigastric and retrosternal region. Heartburn arises in gastro-oesophageal reflux, mostly in the presence of gastric hyperacidity in various diseases of the alimentary tract (e.g. peptic ulcer or cholecystitis), hiatus hernia, and sometimes in pregnancy. Heartburn in healthy subjects can be due to hypersensitivity to some foods.
Nausea, the reflectory act associated with irritation of the vagus nerve, is an indefinite feeling of sickness and sensation of compression in the epigastrium. Nausea is often attended by pallidness of the skin, general weakness, giddiness, sweating, salivation, fall in the arterial pressure, cold in the limbs, and sometimes semisyncopal state. Nausea often (but not necessarily) precedes vomiting. The mechanism of nausea is not known. Its frequent association with vomiting suggests that it might be the early sign of stimulation of the vomiting centre. The leading role in the development of nausea is given to the nervous system and also the tone of the stomach, the duodenum, and the small intestine. Nausea may develop without any connection with diseases of the stomach, e.g. in toxaemia of pregnancy, renal failure, deranged cerebral circulation, and sometimes in healthy people in the presence of foul odour (or in remembrance of something unpleasant). Some diseases of the stomach are attended by nausea, e.g. acute and chronic gastritis or cancer of the stomach. Nausea associated with gastric pathology usually occurs after meals, especially after taking some pungent food. Nausea often develops in secretory insufficiency of the stomach.
Vomiting (emesis) occurs due to stimulation of the vomiting centre. This is a complicated reflex through the oesophagus, larynx and the mouth (sometimes through the nose as well). Vomiting may be caused by ingestion of spoiled food, by seasickness, or irritation arising inside the body (diseases of the gastro-intestinal tract, liver, kidneys, etc.). In most cases vomiting is preceded by nausea and sometimes hypersalivation. Factors causing the vomiting reflex are quite varied. This can be explained by the numerous connections that exist between the vomiting centre (located in the medulla oblongata, in the inferior part of the floor of the 4th ventricle) and all bodily systems. Depending on a particular causative factor, the following can be differentiated: (1) nervous (central) vomiting; (2) vomiting of visceral aetiology (peripheral or reflex); (3) haematogenic and toxic vomiting.
Vomiting is an important symptom of many diseases of the stomach, but it can be regarded as the symptom of a particular disease only in the presence of other signs characteristic of this disease. Vomiting of gastric aetiology is caused by stimulation of receptors in the gastric mucosa by inflammatory processes (acute or chronic gastritis), in ingestion of strong acids or alkalis, or food acting on the gastric receptors by chemical (spoiled food) or physical (overeating or excessively cold food) routes. Vomiting can also be caused by difficult evacuation of the stomach due to spasms or stenosed pylorus.
If the patient complains of vomiting, the physician should inquire about the time when the vomiting occurred, possible connections with
23*
Special Part
Chapter 7. Digestive System


 meals, association with pain, the amount and character of the vomited material. Morning vomiting (on a fasting stomach) with expulsion of much mucus is characteristic of chronic gastritis, especially in alcoholics. Hyperacid vomiting in the morning indicates nocturnal hypersecretion of the stomach. Vomiting occurring 10—15 minutes after meals suggests ulcer or cancer of the cardial part of the stomach, or acute gastritis. If vomiting occurs 2—3 hours after meals (during intense digestion) it may indicate ulcer or cancer of the stomach body. In the presence of ulcer of the pylorus or duodenum, vomiting occurs 4—6 hours after meals. Expulsion of food taken a day or two before is characteristic of pyloric stenosis. Patients with peptic ulcer often vomit at the height of pain thus removing it, which is typical of the disease. The odour of the vomit is usually acid, but it can often be fetid (putrefactive processes in the stomach); the odour may be even faecal (in the presence of a faecal fistula between the stomach and the transverse colon).
meals, association with pain, the amount and character of the vomited material. Morning vomiting (on a fasting stomach) with expulsion of much mucus is characteristic of chronic gastritis, especially in alcoholics. Hyperacid vomiting in the morning indicates nocturnal hypersecretion of the stomach. Vomiting occurring 10—15 minutes after meals suggests ulcer or cancer of the cardial part of the stomach, or acute gastritis. If vomiting occurs 2—3 hours after meals (during intense digestion) it may indicate ulcer or cancer of the stomach body. In the presence of ulcer of the pylorus or duodenum, vomiting occurs 4—6 hours after meals. Expulsion of food taken a day or two before is characteristic of pyloric stenosis. Patients with peptic ulcer often vomit at the height of pain thus removing it, which is typical of the disease. The odour of the vomit is usually acid, but it can often be fetid (putrefactive processes in the stomach); the odour may be even faecal (in the presence of a faecal fistula between the stomach and the transverse colon).
The vomited material may have acid reaction (due to the presence of hydrochloric acid, in hyperchlorhydria), neutral (in achylia), or alkaline (in the presence of ammonia compounds, in pyloric stenosis, hypofunction of renal function, and also in regurgitation of the duodenal contents into the stomach). Vomitus may contain materials of great diagnostic importance, e.g. blood, mucus (in chronic gastritis), ample bile (narrowing of the duodenum, gastric achylia), and faecal matter. Vomiting may attend acute gastritis, exacerbation of chronic gastritis, gastric neurosis, peptic ulcer, spasm and organic stenosis of the pylorus, and cancer of the stomach.
Pain is the leading symptom in diseases of the stomach. Epigastric pain is not obligatory connected with diseases of the stomach. It should be remembered that the epigastrium is the " site of encounter" of all kinds of pain. Epigastric pain may be due to diseases of the liver, pancreas, and due to hernia of the linea alba. Epigastric pain may develop in diseases of other abdominal organs (sometimes of organs located outside the abdomen) by the viscero-visceral reflex (acute appendicitis, myocardial infarction, affection of the diaphragmatic pleura, etc). In order to locate correctly the source of pain, the physician should ask the patient (1) to show exactly the site of pain; (2) to characterize the pain which may be periodical or paroxysmal (at certain time of the day); permanent or seasonal (in spring or autumn); (3) to describe the connection (if any) between pain and meals, the quality of food and its consistency; (4) to indicate possible radiation of pain (into the back, shoulder blade, behind the sternum, left hypochon-drium); (5) to describe conditions under which pain lessens (after vomiting, after taking food or baking soda, after applying hot-water bottle or taking spasmolytics); (6) to describe possible connections between pain and
physical strain (weight lifting, traffic jolting, etc.), or strong emotions. Intensity and character of pain are also important diagnostically. The pain may be dull, stabbing, cutting, etc. Pain in hollow organs with smooth muscles (e.g. stomach) is provoked by spasms (spastic pain), distension of the organ (distensional pain), and by its motor dysfuncion.
Paroxysmal, periodical epigastric pain is due to the spasm of the pyloric muscles. It arises under the influence of strong impulses arriving from the vagus nerve centre in cerebral cortex dysfunction. The spasm of the pylorus is stimulated by the hyperacidity of gastric juice due to hyperstimulation of the vagus. Depending on the time of paroxysmal pain (after meals), it may be early (occurring 30-40 min after meals), late (90-120 min after meals), nocturnal, and hunger pain (which is abated after taking food). If pain occurs after meals stimulating secretion of gastric juice (bitter, pungent, spicy or smoked foods), this indicates the leading role of hypersecretion in its aetiology. The pain then localizes in the epigastrium, radiates to the back, and is rather intense; it is abated after vomiting and taking alkali or foods that decrease acidity of gastric juice, and also after taking antispastic preparations and applying hot-water bottle (which removes spasms).
A seasonal character of pain, i.e. development of periodic pain during spring and autumn, is characteristic of peptic ulcer, especially if the process is localized in the peripyloric region. Permanent boring pain is usually caused by stimulation of the nerve elements in the mucous and submucous layer of the stomach; the pain is usually intensified after meals and is characteristic of exacerbation of chronic gastritis or cancer of the stomach.
Perigastritis (chronic inflammation of the peritoneum overlying the stomach and its adhesion to the neighbouring organs) is manifested by pain developing immediately after taking much food (irrespective of its quality). The full stomach distends to stimulate nerve fibres in the adhesions. In the presence of perigastritis and adhesions between the stomach and the adjacent organs, pain may be caused by any physical strain and when the patient changes his posture.
Gastric haemorrhage is a very important symptom. It can be manifested by vomiting of blood (haematemesis) or by black tarry stools (melaena). Gastric haemorrhage is usually manifested by the presence of blood in the vomitus. The colour of the vomitus depends on the time during which the blood is present in the stomach. If the blood was in the stomach for a long time, the blood reacts with hydrochloric acid of the gastric juice to form haematin hydrochloride. The vomitus looks like coffee grounds. If haemorrhage is profuse (damage to a large vessel) the vomitus contains much scarlet (unaltered) blood. Haematemesis occurs in peptic ulcer, cancer, and polyps, in erosive gastritis, rarely in sarcoma,
Special Part
Chapter 7. Digestive System

 tuberculosis and syphilis of the stomach, and in varicosity of the oesophageal veins. Tarry stools are not an obligatory sign of gastric haemorrhage.
tuberculosis and syphilis of the stomach, and in varicosity of the oesophageal veins. Tarry stools are not an obligatory sign of gastric haemorrhage.
When collecting anamnesis, the patient should be asked about his nutrition. It is important to establish if meals are regular because taking food at random is an important factor in the aetiology of gastric diseases. Food quality is as important as its amount taken during one meal. Mastication of food matters as well. Conditions of rest and work, and possible occupational hazards should be established. Abuse of alcohol and smoking are important factors in the aetiology of gastric diseases. It is very important to find out if the patient's condition has undergone some changes during recent time (e.g. loss of weight, anaemia, blood vomiting, or tarry stools). Gastro-intestinal diseases of the past, surgical intervention on the abdominal organs, long medication with preparations irritating the stomach mucosa (acetylsalycilic acid, sodium salycilate, steroid hormones, potassium chloride, etc.) are also very important.
Physical Examination
,: ■. INSPECTION
During general inspection of the patient the physician may assess poor nutrition of the patient (cachexia) which is characteristic of stomach cancer and untreated benign pyloric stenosis. Pale skin is observed after gastric haemorrhage. Patients with uncomplicated peptic ulcer look practically healthy.
Next stage is inspection of the mouth. The absence of many teeth accounts for inadequate disintegration and mastication of food in the mouth, while the presence of carious teeth favours penetration of micijobial flora into the stomach. The tongue is not the " mirror of the stomach" as it was formerly believed. Nevertheless in some diseases its appearance is informative: clean and moist tongue is characteristic of uncomplicated peptic ulcer, while the tongue coated with a foul smelling white-grey material is characteristic of acute gastritis; a dry tongue indicates a severe abdominal pathology or acute pancreatitis; a tongue with atrophied papillae suggests cancer of the stomach, atrophic gastritis with pronounced gastric secretory hypofuncion, or vitamin B deficiency.
Inspection of the abdomen may give information about the contours and peristalsis of the stomach if the patient is cachectic. In pathological cases (pyloric stenosis), peristalsis can be easily seen (ridges raising the abdominal wall). If the physician rubs or taps on the epigastric region
ristalsis becomes more distinct. Sometimes, in neglected cases, the abdominal wall can be protruded (tumour).
PALPATION
The stomach should be palpated in both the vertical and horizontal position of the patient because the lesser curvature of the stomach and its high standing tumours are impalpable in the lying position. First palpation should be superficial and tentative. Its aim is to establish tenderness of the epigastrium, irritation of the peritoneum (Shchetkin-Blumberg symptom), divarication of the abdominal muscles, the presence of hernia of the linea alba, tension in the abdominal wall in the region of the stomach, and the presence of muscular defence (defense musculaire). Deep palpation of the stomach should be carried out according to Obraztsov and Strazhesko. The examiner pulls up the skin on the abdomen and presses carefully the anterior wall of the abdomen to penetrate the depth until the examining fingers reach the posterior wall. When pressed against the posterior wall of the abdomen, the stomach slips from under the examining fingers. The shape of the stomach and the size of the examined part can thus be assessed. The greater curvature and the pylorus can best of all be examined by this method.
The greater curvature can be examined by deep sliding palpation in 50-60 per cent and the pylorus in 20-25 per cent of healthy subjects; the lesser curvature can be palpated in gastroptosis. The greater curvature is found to either side of the median line, 2—3 cm above the navel. It appears to palpating fingers as a ridge on the back bone and by its sides. In cases with gastroptosis, the greater curvature can descend below the navel. Correctness of determination can be confirmed if the position of the ridge coincides with that of the lower border of the stomach as determined by other techniques (by percussion, by the splashing sound or stethacoustic palpation). The pylorus is located in the triangle formed by the lower edge of the liver to the right of the median line, by the median line of the body, and the transverse line drawn 3-4 cm above the navel, in the region of the right rectus abdominis muslce. Since the position of the pylorus is oblique (upwards to the right) the palpating movements should be perpendicular to this direction, i.e. from left downwards to the right. The pylorus is identified by palpation as a band (tense or relaxed). When the pylorus is manipulated by the fingers, a soft rumbling sound can be heard. When contracted spastically (pylorospasm) the pylorus remains firm for a long time. Sometimes the pylorus is mistaken for cancer infiltration., Palpation of the stomach can reveal tumours of the pylorus, of the
Special Part
Chapter 7. Digestive System



 greater curvature, and of the anterior wall. Tumours of the lesser curvature can be diagnosed with the patient in the upright position. Tumours of the cardial part of the stomach are inaccessible to palpation. Exact information on their location gives X-ray examination.
greater curvature, and of the anterior wall. Tumours of the lesser curvature can be diagnosed with the patient in the upright position. Tumours of the cardial part of the stomach are inaccessible to palpation. Exact information on their location gives X-ray examination.
PERCUSSION
Percussion is used to determine the inferior border of the stomach. Provided professional skill is high, the inferior border of the stomach can be outlined by light percussion by differentiating between gastric and intestinal tympany.
If the patient cannot eat the full meal (the capacity of the stomach gradually decreases), it is necessary to determine the Traube's space, which can be markedly decreased. The presence of these two symptoms requires an X-ray examination to exclude cancer of the stomach (scirrhus). Short strokes of the hammer or the flexed fingers on the epigastrium (Mendel sign) are used to determine involvement of the parietal peritoneum: pain indicates affection of the peritoneum.
Splashing sound (succussion) can be heard if the patient is lying on his back, while the examiner pushes the anterior wall of the peritoneum with four flexed fingers of the apt hand. The other hand of the physician should fix the muscles of the abdominal prelum against the sternal edge. The thrust of the hand is transmitted through the stomach wall to the liquid and air contained inside it to cause a readily audible splashing sound which is inaudible outside the inferior borders of the stomach. This technique for outlining the inferior border of the stomach is effective in cases where the stomach border formed by the greater curvature is at the normal level or lowered. Succussion gives information about the evacuatory function of the stomach: the splashing sounds in healthy subjects can only be heard after meals. Splashing sounds heard 7—8 hours after meals suggest evacuatory dysfuncion of the stomach (mostly in pyloric stenosis) or its pronounced hypersecretion (gastrosuccorrhoea). Splashing sounds heard to the right of the median line of the abdomen indicate dilatation of the prepyloric part of the stomach (Vasilenko's symptom).
AUSCULTATION
Auscultation of the stomach is practically non-informative. It is only helpful when used together with palpation of the stomach to outline its inferior border. Stethacoustic palpation is performed as follows: a
stethoscope is placed beneath the left costal arch, below the Traube's space. The examiner rubs the abdominal wall overlying the stomach by the finger and gradually moves the finger away from the stethoscope bell. As long as the finger rubs the skin overlying the stomach, the physician hears the friction, but when the finger moves outside the stomach borders, the sound disappears. This method is very simple but the findings are sometimes inaccurate.
Laboratory and Instrumental Methods
EXAMINATION OF THE SECRETORY FUNCTION
Study of gastric secretion is an indispensable part of complex diagnosis of the gastric mucosa function. The most reliable data on the gastric secretion can be obtained by studying gastric juice.
A thick tube was used for many years to study gastric secretion. The main disadvantage of this method is that a mixture of gastric juice and test meal is extracted and it is thus impossible to obtain reliable qualitative and quantitative characteristics of gastric secretion. This method can therefore be considered obsolete.
Adequate probing implies obtaining pure gastric juice and studying gastric secretion for long periods of time, during various periods of the secretory cycle. Information about gastric juice must be not only qualitative but also quantitative. In other words, probing must give maximum information about the condition of gastric mucosa. Suitable agents stimulating secretion of gastric juice should be used for the purpose. In order to follow-up gastric secretion a thin tube is used.
This is an elastic rubber tube with the outer diameter of 4-5 mm and the inner diameter 2—3 mm. The blind end has two lateral openings. Since the tube is elastic and soft, it is impossible to introduce it in the oesophagus by force (as is the case with a thick tube). The patient has to swallow it gradually. If the vomiting reflex arises, the tube can be introduced through the nose. When the tube reaches the stomach it no longer provokes vomiting and may be left in the stomach for more than two hours. The stomach contents can thus be withdrawn at any suitable time and the secretory gastric function can thus be assessed not at a single moment but can be followed up for considerable length of time. A syringe attached to the free end of the tube is used to suck off the stomach contents.
The study usually begins with removal of gastric juice from a fasting stomach. This done, an agent stimulating gastric secretion can be introduced. According to other methods, from two to four 15-minute samples of the juice are taken from the fasting stomach. This is the so-called basal secretion, though the term does not exactly define the essence of the pro-
Special Part
Chapter 7. Digestive System

 cess, because it is very difficult to decide whether the obtained juice is spontaneous secretion or secretion induced by the swallowing movements, or the tube itself.
cess, because it is very difficult to decide whether the obtained juice is spontaneous secretion or secretion induced by the swallowing movements, or the tube itself.
After the last (fourth) portion of the basal secretion is obtained (in 60 min), the patient is given a stimulating agent (test meal), which may be given either through the gastric tube or parenterally (pentagastrin, histamine, insulin). Pentagastrin (synthetic) and histamine are very effective; these are physiological stimulants of gastric secretion. Histamine is contraindicated in organic cardiovascular diseases, allergic diseases, high arterial pressure, phaeochromocytoma, and after recent (2—3 weeks ago) gastro-intestinal haemorrhage. The dose of histamine is calculated according to the patient's weight (0.01 mg per kg body weight). This stimulation of gastric secretion is submaximal. There exists an optimum (maximum) dose of histamine: a further increase of the dose does not intensify secretion of the stomach (0.04 mg of histamine phosphate per kg body weight). If the maximum dose of histamine is given (Kay's test), the patient should first be given an antihistamine preparation.
After administration of histamine or pentagastrin, gastric juice is collected for an hour, at 15-minute intervals.
There exist many enteral stimulants of gastric secretion. These are beaf tea, a 5 per cent alcohol solution, caffeine (0.2 g in 300 ml of water), a 7 per cent decoction of dry cabbage, etc. They are given to patients to whom histamine is contraindicated.
If stimulants of gastric secretion are given per os, gastric juice is obtained by the Leporsky method. After extraction of four portions of the basal secretion, 300 ml of cabbage decoction (20 titration units) are given into the stomach through the tube. First a 10-ml specimen is taken in 10 minutes, and then, in 15 minutes, the entire stomach contents are aspirated. Four other 15-minute portions are then taken which contain pure gastric juice excreted by the stomach in response to the removed stimulant. Each juice specimen is collected in a separate vessel and its quantity is marked. A fasting stomach of a healthy individual contains to 50 ml of the fluid; sometimes this amount is larger. An hourly basal secretion is 30—150 ml (50 ml on the average). The evacuating function of the stomach is determined by the volume of gastric juice contained in it 25 minutes after a test meal. The normal volume is 75 ml, on the average. Summation of the last four portions gives the hourly secretion. A 15-minute portion (with intermittent aspiration) is not quite informative because part of gastric juice passes into the duodenum. A continuous aspiration of gastric juice (with separation of 15-minute portions) ensures more accurate determination of hourly secretion. Normally it is about 60 ml with intermittent aspiration, while with continuous aspiration this figure increases 1.5—2 times. If
parenteral stimulants are used, gastric juice is aspirated for 60 minutes straight after their administration.
The colour of the extracted juice, its consistency, the presence of admixtures, and odour are assessed. Normal gastric juice is almost colourless. Bile (that may be belched into the stomach from the duodenum) colours the juice green or yellow; blood admixtures give the juice a red colour, or (more frequently) brownish-black. If much unaltered scarlet blood is aspirated together with juice probing should be discontinued immediately. Normal juice is liquid; the presence of mucus makes it tenacious and it is sometimes difficult to separate a portion from the whole mass of the juice taken. Ample mucus in the juice may suggest gastritis. Supernatant mucus originates from the airways. Residues of food taken the day before the examination may also be present in gastric juice. This indicates motor dysfunction of the stomach.
After the physical properties of gastric juice have been determined, its chemical properties should be established. Free hydrochloric acid is first determined in each sample; next determined are bound hydrochloric and lactic acid; pepsin is determined in the sample with maximum acidity.
Acidity of gastric juice is determined by titrating it with a 0.1 N sodium hydroxide solution in the presence of indicators. Acidity is expressed in millilitres of NaOH which are spent to neutralize 100 ml of the juice. It has become usual now to express acidity in milligrams of HC1 or milli-equivalents (MEq). Two drops of a 0.5 per cent alcoholic solution of dimethylamidoazobenzene and two drops of a 1 per cent alcoholic solution of phenolphthalein (phenol red is now very popular) are added to a 5- or 10-ml aliquot. Dimethylamidoazobenzene turns red in the presence of free HC1. Alkali is buretted, drop by drop, to the gastric juice until it turns pinky orange to indicate the point of equivalence. The amount of the alkali spent is determined and titration is continued. The liquid first turns yellow and then red again: all acid has been neutralized and phenolphthalein turns red. The new spent volume of alkali is measured again. The number of millilitres of the alkali that were spent at the first stage of titration are multiplied by 20 to give the amount of free hydrochloric acid. The amount of alkali spent for the entire titration should also be multiplied by 20 to determine total acidity. This is the sum of all acids contained in the stomach, e.g. free and bound hydrochloric acid, organic acids, and acid phosphates. Bound acid is non-dissociated hydrochloric acid of protein hydrochloride molecules of gastric juice. Normal gastric juice contains proteins (pepsin, gastromucoprotein). The protein content increases in gastritis, bleeding ulcer, or degradation of a tumour; the amount of bound hydrochloric acid increases accordingly. Bound acid is determined indirectly by titrating a small (5 ml) portion of the juice in the presence of alizarin
Special Part
Chapter 7. Digestive System

 sodium sulphonate which is yellow in the presence of any free acid. When acid is neutralized, the solution turns violet. Bound HCl is determined by subtracting the number of millilitres of alkali spent for titration with alizarin from total acidity and multiplying the difference by the factor of 20. Indices of acidity that were considered to be normal for decades have now been revised. Thus the normal content of hydrochloric acid in the fasting stomach of a healthy subject was considered to be maximum 10-20 titrating units (t.u.), or the acid might be absent at all. Normal acidity after taking a test meal was 20-40 titrating units for free HCl and 40-60 for total acidity. Findings of many investigators who observed a great number of healthy people show that " normal" acidity is found in only 50 per cent of them, while in others acidity is either below or above this " normal" level and is their constitutional feature. Total acidity below 20 t.u. should therefore be considered hypo-acidity and over 100 t.u. hyperacidity. Complete absence of hydrochloric acid is a very important diagnostic sign. The absence of free HCl in gastric juice after giving the maximum dose of histamine is called histamine refractory achlorhydria. This symptom may suggest atrophic process in gastric mucosa.
sodium sulphonate which is yellow in the presence of any free acid. When acid is neutralized, the solution turns violet. Bound HCl is determined by subtracting the number of millilitres of alkali spent for titration with alizarin from total acidity and multiplying the difference by the factor of 20. Indices of acidity that were considered to be normal for decades have now been revised. Thus the normal content of hydrochloric acid in the fasting stomach of a healthy subject was considered to be maximum 10-20 titrating units (t.u.), or the acid might be absent at all. Normal acidity after taking a test meal was 20-40 titrating units for free HCl and 40-60 for total acidity. Findings of many investigators who observed a great number of healthy people show that " normal" acidity is found in only 50 per cent of them, while in others acidity is either below or above this " normal" level and is their constitutional feature. Total acidity below 20 t.u. should therefore be considered hypo-acidity and over 100 t.u. hyperacidity. Complete absence of hydrochloric acid is a very important diagnostic sign. The absence of free HCl in gastric juice after giving the maximum dose of histamine is called histamine refractory achlorhydria. This symptom may suggest atrophic process in gastric mucosa.
Acidity (concentration of the acid) does not characterize completely the acid-secreting function of the stomach. A more detailed information can be obtained by determining the hourly secretion of the stomach. To that end, acid concentration in the gastric juice should be multiplied by the hourly secretion of the stomach and divided by 100 (if acid concentration is expressed in mg/100 ml) or by 1000 (if the concentration is given in mEq/1).
Acidity in titration units can be expressed as concentration of the acid in mg/100 ml by multiplying the acidity index by 3.65, because the weight equivalent of the titration unit is 3.65 mg HCl or 0.1 mEq HCl in 100 ml of gastric juice. For example, acidity of 60 t.u. can be expressed as (3.65 x 60) mg/100 ml or 60 mEq/1, or 60 mmol/1 HCl. Indices of gastric secretion for various phases and with various stimulants are given in the Appendix.
Since probing is contraindicated to some patients (with degrading tumour of the stomach, stenosis of the oesophagus, aortic aneurysm, etc.), and since some patients fail to swallow the gastric tube, many investigators search for techniques by which acidity of the gastric secretion can be determined without using any tubes. In 1905, Sahli suggested a simple method. The patient swallows a small rubber bag (tied up with catgut) containing 0.1 g of methylene blue and has a normal meal. If hydrochloric acid is present in the stomach, catgut is digested and methylene blue is absorbed in the stomach contents to colour urine later. Methods employing ion-exchange resins have been recently proposed. Ion-exchange pills contain
substances that are displaced from them by hydrochloric acid in the stomach and then excreted in the urine. Quinine, stains (azur I) and other substances are used in such pills. These methods are quite reliable but they can only determine complete absence or presence of the acid in the stomach and cannot give quantitative information. Moreover, these methods are applicable to patients with preserved renal function.
A new and promising radiotelemetric method is now used to determine acidity (to be more exact, the pH) of gastric juice. This method is known as endoradioprobing.
Another important property of gastric juice is its peptic power. It is determined mostly by the extent to which protein is digested.
The simplest method of establishing peptic activity of gastric juice was proposed in 1899 by Mett. Narrow glass tubes filled with coagulated egg white are immersed in gastric juice (which is acidified, if free HCl is absent) and then placed in a thermostat for 24 hours. The length of tubes (in mm) freed from the albumen is measured. If pepsin content is normal, the total number of millimetres (on both ends of the tube) should be 6-12.
V. Tugolukov proposed a standard method by which more accurate results can be obtained. A 2 per cent solution of dry plasma is placed in two accurately graduated centrifugal tubes and gastric juice in question (diluted 1: 100) is added. A portion of boiled juice is added to one test tube and both are kept in a thermostat for 20 hours. Trichloracetic acid is then added to the test tubes, the contents are mixed thoroughly, and the solutions are cen-trifuged. The peptic power of gastric juice is assessed by the volume of precipitated albumin. The findings are compared with the results of similar experiments carried out with pure dry pepsin of different dilutions. The pepsin content of gastric juice can thus be expressed in milligrams.
If the pepsinogenic function of the stomach is estimated without probing, pepsinogen is determined in the urine (uropepsinogen). It has been established that pepsin is not fully secreted into the stomach, but about 1 per cent of it is mixed with blood and liberated with urine. The presence of pepsinogen in the urine therefore indicates its secretion by the gastric mucosa. Uropepsinogen is determined in the same way as pepsin in gastric juice; Tugolukov's method (or milk coagulation method) can also be used for the purpose.
Determination of lactic acid in gastric juice has a certain diagnostic importance as well. The acid is produced either by the lactobacillus, which grows in the stomach only in the absence of hydrochloric acid, or by a malignant tumour: anaerobic glycolysis occurs in its cells with formation of lactic acid. The presence of lactic acid in gastric juice is not pathognomonic for tumour, but requires a thorough examination of the patient. Uffelmann reaction is used for determining lactic acid. A 1—2 per
Special Part
Chapter 7. Digestive System

 cent phenol solution is placed in a test tube (2/3 full capacity) and 2-3 drops of a 10 per cent ferric chloride solution added: the reagent turns dark-violet. The test tube is then inclined and 2—3 drops of gastric juice are added by the wall. In the presence of lactic acid, the drops of juice sink to the bottom and become coloured bright-yellow by the iron lactate formed.
cent phenol solution is placed in a test tube (2/3 full capacity) and 2-3 drops of a 10 per cent ferric chloride solution added: the reagent turns dark-violet. The test tube is then inclined and 2—3 drops of gastric juice are added by the wall. In the presence of lactic acid, the drops of juice sink to the bottom and become coloured bright-yellow by the iron lactate formed.
Microscopic studies. Native preparations are made from a settled or centrifuged precipitate. Gastric juice precipitate of healthy subjects contains mostly cells of the mouth (squamous epithelium and leucocytes). The presence of food remains (muscle fibres, fat, fatty acids, subcutaneous fat) indicates evacuation dysfuncion of the stomach. Acid stagnant juice contains sarcinae. If acidity is absent, lactic bacilli are present in the juice. Erythrocytes in small quantities are diagnostically unimportant because their presence may be due to an injury caused by probing or strain during vomiting. Ample erythrocytes suggest the presence of ulcer, tumour, or erosive gastritis.
Exfoliative cytology. Early cancer of the stomach, when the tumour cannot be palpated and revealed by X-ray, is difficult to diagnose. Exfoliative cytology is a simple method by which tumour of the stomach can be established to a high degree of certainty. The method is based on the specific property of cancer cells to be easily separated from one another and shed into gastric contents. The cells are recovered from the precipitate or the gastric washings. Special gastric tubes with inflated bulbs which have rough surface to separate cancer cells are used to obtain desquamated cells. In order to prevent degradation of cancer cells, the obtained gastric juice should be immediately centrifuged and the precipitate examined either in native preparations or in a phase-contrast microscope after staining with fluorochromes, or in dry smears stained by haematoxylin-eosin, or after Romanowsky-Giemsa or Papanicolaou. Differentiation of gastric tumour cells requires great experience, because they are very much like cells of other tumours (see " Study of Sputum").
STUDY OF GASTRIC MOTOR FUNCTION
The motor function of the stomach is assessed by its peristole, peristalsis (of a fasting stomach and after meals), intragastric pressure, and the evacuatory function. Various methods exist to study these characteristics, e.g. inquiry of the patient, physical examination, balloon kymography, electrogastrography, radiotelemetry, and roentgenography. It should be noted that none of them can give exhaustive characteristic of the motor function of the stomach. At the same time, each method adds to the picture of this complicated process.
Balloon kymography. The movements of the stomach and the height of its peristalsis are recorded on a moving paper chart by a kymograph employing a float. The variables are picked up by a single- or a multichannel gastric tube ending with balloons (sensitive elements) which is swallowed by the patient. The fasting stomach is thus examined. The position of the balloon in the stomach is controlled by X-rays.
The following regularities of a fasting stomach in healthy individuals have been established: the stomach " works" from 10 to 40 minutes, and then a period of relative rest, lasting from 40 to 120 minutes, follows. The height of waves on a gastrogram varies from 3 to 6 cm, while the number of contractions per minute is 1 or 2 on the average. Pressure in the stomach body varies from 6 to 10 cm H2O. The contraction frequency in the pyloric part of the stomach is higher (2—3 contractions per minute); the waves are higher too (to 7 cm).
Electrogastrography. This is the method of recording biopotentials characterizing the motor function of the stomach. Electrogastrography is the best method to record digestive peristalsis of the stomach. Since action currents are taken off from the surface of the human body, no tube should be swallowed. The absence of the tube inside the stomach, in turn, does not interfere with its normal secretory function. When a tube is swallowed, it may happen that food gets between the electrode and the stomach wall to break contact. This distorts intragastric records or makes recording unfeasible at all.
The active electrode is placed on the median line of the abdomen, below the xiphoid process, at the point of projection of the antral end of the stomach. The other electrode is placed on the right leg of the patient. An electrogastrogram is recorded after giving a test meal (150 g of wheat bread and a cup of sweet tea). The most distinct peristalsis of the stomach is recorded in 30-120 minutes after the test meal. When interpreting the ECG, the general character of the curve, the amplitude and frequency of waves, and the peristaltic rhythm are assessed. The amplitude of waves on an ECG of a healthy individual does not exceed 1/4 mV and only some amplitudes are 0.5 or 1 mV. The rhythm of oscillations is three per minute. Electrogastrography is of little use in differential diagnosis of affections of digestive organs, but it can help assess objectively effects of various pharmacological and other factors on gastric peristalsis during digestion, and follow up changes in the motor function of the stomach during treatment.
Endoradioprobing. The operating principle of this radiotelemetric study is recording of signals emitted from an ingested miniature transmitter (endoradioprobe) that responds to physiological, physical, and chemical changes occurring inside the digestive tract. Endoradioprobe consists of a transmitter and a sensitive element (made in the form of a cylinder) which responds to changes in the controlled variable (pressure pH, temperature) and generates high-frequency electromagnetic oscillations. The emitted signals are received and recorded. A flexible aerial transmits the signals. It is enclosed in a silk belt attached to the patient's body. A special calibrating device is provided to ensure high accuracy of measurement of physiological parameters. The transmitter is introduced into the patient's stomach together with a thin gastric tube which is usually used for taking gastric juice specimens. The probe has openings at its lower end to aspirate the contents of the stomach or the duodenum. Depending on the object of study, the tube may be introduced into a fasting stomach or after taking a test meal. The patient assumes the recumbent position.
The radio transmitter can also be used to study gastric secretion, evacuatory function of the stomach, and effect of various pharmacological preparations, and to record variations in pressure inside the stomach.
X-RAY STUDY
Roentgenoscopy and roentgenography are important methods for examination of the stomach. They are used to outline the shape, size, position, and mobility of the stomach, and to locate its ulcers or tumours.
Special Part
Chapter 7. Digestive System
1 I
Relief of the gastric mucosa and its functional conditions can also be determined roentgenologically.
An empty stomach is examined with a barium meal as a contrast substance (100-150 g of barium sulphate in a cup of water).
In the presence of hypersecretion or evacuatory dysfunction the stomach of the patient may contain considerable quantity of material. This should be removed through a tube before giving the barium meal. The patient is then asked to swallow one or two mouthfuls of barium sulphate suspension. By palpating the anterior wall of the abdomen, the suspension is distributed by the surface of the gastric mucosa to fill its folds: gastric mucosa becomes visible on an X-ray screen. The direction of the folds, their thickness, continuity, thickness height, and elasticity should be assessed. After the relief of the gastric mucosa has thus been examined, the patient is asked to drink the remaining meal to fill the stomach so that its shape, size, position, general outline, mobility, evacuation function, possible affections, and the condition of the gastric gas bubble might be examined. During examination, the patient is asked to turn before the screen in both horizontal and vertical planes. Whenever necessary, X-ray pictures are made. In order to study the motor function of the stomach a series of pictures are taken (roentgenocinematography).
Folds of gastric mucosa are longitudinal in the region of the lesser curvature, and oblique in the region of the greater curvature. The folds in the region of the antrum can be seen to extend in both directions. The shape of the folds is important: they may be broad and rough; or they may be absent (in atrophied mucosa). Continuity of the folds should be established: if the folds disappear, the presence of pathology may be suggested at this site (e.g. cancer, or other process destroying the gastric mucosa).
When the stomach is full, it resembles a hook located in the upper portion of the abdominal cavity, to the left of the median line. The shape of the stomach can change significantly in pathology, e.g. it can look like a bag in decreased tone, or resemble a sand glass in the presence of cicatricial adhesions.
The stomach outlines are of great diagnostic importance. Permanent protrusion of the stomach silhouette (niche) is a direct indication of gastric ulcer. If barium sulphate fails to fill any portion of the stomach a filling defect forms; it may suggest a tumour. Peristaltic movements of the stomach alter its contours, but as distinct from organic changes in the stomach wall, they are only transient.
The evacuatory function of the stomach is characterized by the time which is necessary for the stomach to discharge the barium meal. Normally, one third of the taken suspension may be present in the stomach in an hour.
The position of the stomach is also very important. The upper pole of a
normal stomach is at the level of the 11-12th thoracic vertebrae; the pylorus is at the level of the 3rd lumbar vertebra; and the lower point (sinus) at the level of the 3rd and 4th vertebrae (not below this level).
GASTROSCOPY
Gastroscopy is inspection of the stomach by a gastroscope. This instrument is similar in design to all other endoscopes. Fibroscopes have recently come in wide use. These are flexible gastroscopes in which the picture is transmitted through a bundle of glass fibres (as thin as a human hair). Another novelty in gastroscopy is taking tissue samples under visual control, and taking pictures and filming of the gastric mucosa. As distinct from common gastroscopes, gastrofibroscopes are flexible and much more convenient for use. Safety of the new instrument is another important factor.
Gastroscopy of a fasting stomach is carried out in the morning. An injection of atropine sulphate (0.001 g) is given to the patient 30 minutes before the procedure. The pharynx and the upper oesophagus are anaesthetized by a 3 per cent dicaine solution. A gastroscope is then introduced following special instructions.
As viewed through a gastroscope the mucosa of the stomach may be pale-crimson to red. The mucosa of the anterior' wall is smooth and covered with a thin glassy layer of mucus (its folds are stretched by the inflating air). Big folds and interconnecting ridges can be seen on the posterior wall of the stomach. The pylorus appears as a cone-shaped structure. The antrum looks like a funnel with its narrow part being directed toward the pylorus. When opened, the pylorus looks like a dark cavity; when the stomach muscles contract, the folds are converged to make a stellar pattern.
Gastroscopy is an important procedure since the condition of the gastric mucosa can be visualized: its colour, minutest changes in the surface, growths, erosions, and ulcers (Plate 12). Gastroscopy reveals the condition of the vessels, haemorrhages, and formation of mucus. It can be used to study the relief of the inner surface of the stomach, i.e. height, width, and density of folds, which is an important supplement to the X-ray examination. Gastroscopy helps reveal tumours or ulcers that were not identified by roentgenoscopy. Gastric mucosa can be filmed through a gastroscope using a special photographic attachment (Fig. 85).
A comprehensive X-ray examination of the patient should be done before gastroscopy in order to reveal possible contraindications (narrowing of the oesophagus or cardia due to a tumour; diverticula of the oesophagus; affections of the mediastinum, which displace the
24-1556
Special Part
Chapter 7. Digestive System

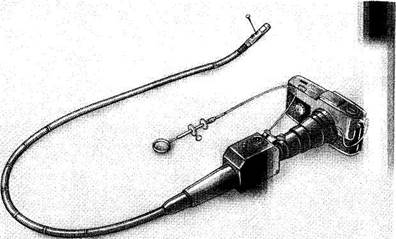
Fig. 85. Gastroscope.
|
|