
Главная страница Случайная страница
Разделы сайта
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Increased pressure in the left atrium increases pressure in the pulmonary veins and this in turn causes reflex contraction of the arterioles 1 страница
|
|

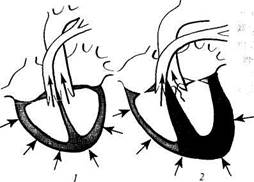
Fig. 69. Changes in the intracardiac haemodynamics in mitral incompetence.
^—normal heart; 2—heart with mitral incompetence (the hypertrophied chambers are printed in red; normal
blood flow is shown by straight arrows, and the regurgitated flow is shown by the wavy arrow).
Special Part
Chapter 6. Blood Circulatory System


 in the lesser circulation (Kitaev's reflex) due to stimulation of barorecep-tors. Spasm in the arterioles increases significantly pressure in the pulmonary artery to intensify the load on the right ventricle which has to contract with a greater force in order to eject blood into the pulmonary trunk. The right ventricle can therefore also be hypertrophied during longstanding pronounced mitral incompetence.
in the lesser circulation (Kitaev's reflex) due to stimulation of barorecep-tors. Spasm in the arterioles increases significantly pressure in the pulmonary artery to intensify the load on the right ventricle which has to contract with a greater force in order to eject blood into the pulmonary trunk. The right ventricle can therefore also be hypertrophied during longstanding pronounced mitral incompetence.
Clinical picture. Most patients with mild or moderate mitral incompetence have no complaints for a long time and look very much like healthy subjects. As congestion in the lesser circulation develops, dyspnoea, palpitation of the heart, cyanosis, and other symptoms appear.

|
|
Palpation of the heart area reveals displacement of the apex beat to the left and sometimes inferiorly. The beat becomes diffuse, intensified, and resistant, which indicates hypertrophy of the left ventricle. Percussion reveals displacement of the heart's borders to the left and superiorly because of the enlarged left atrium and left ventricle. The configuration of the heart becomes mitral with an indistinct heart waist. The border of the heart shifts to the right in hypertrophy of the right ventricle. Auscultation of the heart reveals decreased first sound at the heart apex because the valves never close completely in this disease. Systolic murmur can be heard at the same point, which is the main sign of mitral incompetence. It arises during systole when the stream of blood passes a narrow slit leading from



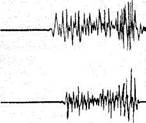
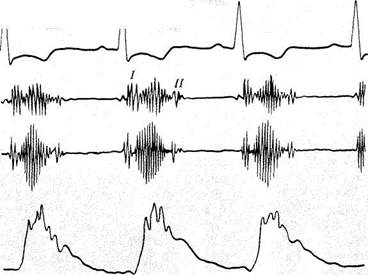
Fig. 70. PCG in mitral incompetence. The amplitude of the first sound is decreased on a PCG taken at the heart apex; systolic murmur occupies the entire pause between the first and second
heart sounds.
the left ventricle to the left atrium. The systolic murmur is synchronous with the first sound. When the blood pressure rises in the lesser circulation, an accent of the second sound can be heard over the pulmonary trunk.
Auscultation findings are confirmed and verified by phonocar-diography (Fig. 70). The pulse and arterial pressure do not change in com-" pensated mitral incompetence. X-ray studies show a specific enlargement of the left atrium and the left ventricle detectable by enlargement (to the left, superiorly and posteriorly) of the heart silhouette. When blood pressure increases in the lesser circulation, the pulmoanry arch dilates. Signs of hypertrophy of the left atrium and the left ventricle can also be found on the ECG: it becomes the left type and the P waves become higher.
Echocardiography reveals distention of the left heart chambers (atrium and ventricle), movement of the mitral valve cusps in the opposite direction, their thickening and the absence of full closure during systole.
Mitral incompetence may remain compensated for a long time. But a long-standing pronounced mitral incompetence and decreased myocardial contractility of the left atrium and the left ventricle cause venous congestion in the lesser circulation. Contractility of the right ventricle can later be affected with subsequent development of congestion in the greater circulation.
STENOSIS OF THE LEFT ATRIOVENTRICULAR ORIFICE
The left atrioventricular orifice usually narrows in a long-standing rheumatic endocarditis (stenosis ostii venosi sinistri). In very rare cases mitral stenosis may be congenital or secondary to septic endocarditis. The atrioventricular orifice narrows due to adhesion of the mitral cusps, their consolidation and thickening, and also shortening and thickening of the tendons. The valve thus becomes a diaphragm or a funnel with a slit in the middle. Cicatricial and inflammatory narrowing of the valvular ring is less important in genesis of mitral stenosis. The valve may be calcified in longstanding stenosis.
If stenosis is significant and the orifice is narrowed from the normal 4-6 cm2 to 1.5 cm2 and less, haemodynamics becomes affected considerably. During diastole, blood fails to pass from the left atrium to the left ventricle and the remaining blood is added to the blood delivered from the pulmonary veins. The left ventricle thus becomes overfilled with blood, the pressure in the ventricle increases. Excess pressure is first compensated for by intensified contraction of the atrium and its hypertrophy, but the force of the left atrial muscle is insufficient to compensate permanently for the pronounced narrowing of the mitral orifice and its contractile force soon weakens; the atrium becomes dilated, and the pressure inside it rises. This in turn increases pressure in the pulmonary veins, produces a reflex
Special Part
Chapter 6. Blood Circulatory System



 spasm in the arterioles of the lesser circulation and increases pressure in the pulmonary artery. All this requires intensified work of the right ventricle, which later also becomes hypertrophied. The left ventricle in mitral stenosis receives smaller volumes of blood and is therefore less active; its size slightly decreases (Fig. 71).
spasm in the arterioles of the lesser circulation and increases pressure in the pulmonary artery. All this requires intensified work of the right ventricle, which later also becomes hypertrophied. The left ventricle in mitral stenosis receives smaller volumes of blood and is therefore less active; its size slightly decreases (Fig. 71).
Clinical picture. When congestive changes occur in the lesser circulation, the patient develops dyspnoea and palpitation on physical exertion; he complains of pain in the heart, cough, and haemoptysis. Inspection reveals acrocyanosis and cyanotic blush on the face. If the disease develops in childhood, the patient's physical growth often slows down and infantilism may develop (" mitral nanism")- Visual examination of the heart region often reveals a cardiac beat consequent upon dilatation and hypertrophy of the right ventricle. The apex beat is not intensified; its palpation can reveal diastolic cat's purr (presystolic thrill). The broadening of cardiac dullness to the right and superiorly due to hypertrophy of the left atrium and right ventricle can be determined by percussion. The heart becomes " mitral" in configuration.
| Fig. 71. Changes in the intracardiac haemodynamics in mitral stenosis. The wavy arrow indicates an obstructed passage of blood from the atrium to the ventricle (for designations see Fig. 69). |
In auscultation of the heart the first sound at the apex becomes loud and snapping because the left ventricle receives little blood and its contraction is fast. An adventitious sound due to the opening of the mitral valve can be heard at the apex beat. It follows the second sound of the heart. The loud first sound, second sound, and the sound of mitral valve opening give a specific murmur which is characteristic of mitral stenosis. The second sound becomes accentuated over the pulmonary trunk when pressure in the lesser circulation increases. Diastolic murmur is characteristic of mitral stenosis because the passage from the left atrium to the ventricle during diastole is narrowed. This murmur can be heard to follow the mitral valve

opening sound (protodiastolic murmur) because the velocity of the blood flow in early diastole is higher due to the pressure difference in the atrium and the ventricle. The murmur disappears when the pressures equalize. If stenosis is not pronounced, the murmur can be heard only at the end of diastole, immediately before systole proper (presystolic murmur); it arises during acceleration of the blood flow at the end of ventricular diastole because of the early atrial systole. Diastolic murmur can be heard in mitral stenosis during the entire diastole. It increases before systole and joins the first snapping sound.
The pulse in mitral stenosis may be different on the left and right arms. In considerable hypertrophy of the left atrium, the left subclavian artery is compressed and the pulse on the left arm becomes smaller (pulsus dif-ferens). If the left ventricle is not filled completely and the stroke volume is decreased, the pulse becomes small (pulsus parvus). Mitral stenosis is often complicated by atrial fibrillation, and the pulse becomes arrhythmic. Arterial pressure usually remains normal; the systolic pressure sometimes slightly decreases and diastolic pressure increases. X-ray patterns of the heart show the specific enlargement of the left atrium, which leads to disappearance of the heart waist and " mitral" configuration appears (Fig. 72a). Enlargement of the left atrium is determined in the first oblique position by the degree of displacement of the oesophagus which becomes especially vivid with barium sulphate suspension (Fig. lib). If pressure in the lesser circulation increases, X-rays show swelling of the pulmonary arch and hypertrophy of the right ventricle. X-ray pictures sometimes show calcification of the mitral valve. Pneumosclerosis develops during longstanding hypertension of the lesser circulation; it may also be revealed during X-ray examination.
The ECG of the heart with mitral stenosis shows hypertrophy of the left atrium and the right ventricle: the amplitude and duration of the P wave increase, especially in the first and second standard leads; the electrical axis of the heart deviates to the right, a high R wave appears in the right chest leads and a pronounced S wave in the left chest leads.
A phonocardiogram taken at the apex shows the high amplitude of the first sound; the second sound is followed by the mitral valve opening sound and diastolic murmur; the amplitude of the second sound over the pulmonary artery increases compared with that over the aorta (Fig. 73). If PCG and ECG are taken synchronously, attention should be paid to the length of the interval Q-\ sound (from the beginning of the Q wave on the ECG to the first sound on the PCG) and the second sound— OS interval. Echocardiograms in mitral stenosis are characterized by the following:
1. The A wave, describing the maximum opening of the valve during atrial systole either decreases or disappears altogether.
Special Part
Chapter 6. Blood Circulatory System

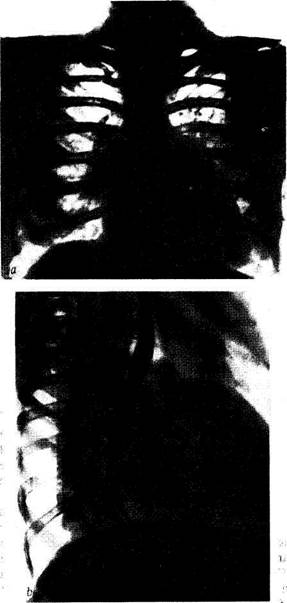
Fig. 72. X-ray of a heart with mitral stenosis.
a—mitral heart; b —deviation of the contrasted oesophagus by the small radius arc in the right anterior oblique position.

Fig. 73. PCG in mitral stenosis. The PCG taken at the heart apex shows increased amplitude of the first sound, diastolic (presystolic) murmur, and the sound of the mitral valve opening
(OS).
2. The speed of diastolic closure of the anterior mitral cusps decreases
to decrease the E-F slope.
3. Movements of the cusps change. The cusps of a normal mitral valve
move in the opposite direction to set apart during diastole: the anterior
cusp moves toward the anterior wall while the posterior cusp to the
posterior wall. In stenosis, these movements become unidirectional because
the more massive anterior wall pulls the posterior one by adhesion. The
movement of the valve is represented on the echocardiogram in the form of
a square wave. Enlargement of the left atrium and changes in the cusps
(fibrosis, calcinosis) can also be detected by echocardiography.
Mitral stenosis soon becomes attended by congestion in the lesser circulation which requires greater work of the right ventricle. Decreased contractility of the right ventricle and venous congestion in the greater circulation develop therefore in mitral stenosis earlier and more often than in mitral incompetence.
. Dilatation of the right ventricle and weakening of its myocardium are sometimes attended by relative tricuspid insufficiency. Moreover, long-
Special Part
Chapter 6. Blood Circulatory System
 standing venous congestion in the lesser circulation in mitral stenosis causes, with time, sclerosis of the vessels and growth of connective tissue in the lungs. Another obstacle to the blood flow is thus created in the lesser circulation and this adds to the difficulties in the work of the right ventricle.
standing venous congestion in the lesser circulation in mitral stenosis causes, with time, sclerosis of the vessels and growth of connective tissue in the lungs. Another obstacle to the blood flow is thus created in the lesser circulation and this adds to the difficulties in the work of the right ventricle.
AORTIC INCOMPETENCE
Aortic incompetence (aortic insufficiency) is the failure of the aortic valve to close completely during ventricular diastole; blood thus leaks back into the left ventricle. Aortic incompetence is usually secondary to rheumatic endocarditis, and less frequently bacterial (septic) endocarditis, syphilitic affection of the aorta, or atherosclerosis. Inflammatory and sclerotic changes occurring in the base of the cusps during rheumatic endocarditis make them shrink and shorten. Atherosclerosis and syphilis can affect only the aorta (to distend it), while the valve cusps are only shortened. The cicatricial changes may extend onto the cusps to disfigure them. Parts of the valve disintegrate in ulcerous endocarditis associated with sepsis and the cusps are affected with their subsequent cicatrization and shortening.

|
| Fig. 74. Changes in the intracardiac haemodynamics in aortic incompetence. The hyper-trophied chambers are printed in red (for designations see Fig. 69). |
Haemodynamics. During diastole, blood is delivered into the left ventricle not only from the left atrium but also from the aorta due to regurgita-tion, which overfills and distends the left ventricle during diastole. During systole, the left ventricle has to contract with a greater force in order to ex-pell the larger blood volume into the aorta. Intensified work of the left ventricle causes its hypertrophy, while the increased systolic volume in the aorta causes its dilatation (Fig. 74).
Aortic incompetence is characterized by a marked variation in the blood pressure in the aorta during systole and diastole. An increased volume of blood in the aorta during systole increases systolic pressure and since part of blood is returned during diastole into the ventricle, the diastolic pressure quickly drops.
Clinical picture. Subjective condition of patients with aortic incompetence may remain good for a long time because the defect is compensated for by harder work of the powerful left ventricle. Pain in the heart (anginal in character) may sometimes be felt; it is due to relative coronary insufficiency because of pronounced hypertrophy of the myocardium and inadequate filling of the coronary arteries under low diastolic pressure in the aorta. The patient may sometimes complain of giddiness which is the result of deranged blood supply to the brain (which is also due to low diastolic pressure).
If contractility of the left-ventricular myocardium is impaired, congestion in the lesser circulation develops and the patient complains of dyspnoea, tachycardia, weakness, etc. The skin of the patient is pallid due to insufficient filling of the arterial system during diastole. Marked variations in the pressure in the arterial system during systole and diastole account for the appearance of some signs, such as pulsation of the peripheral arteries, the carotids (carotid shudder), subclavian, brachial, temporal, and other arteries; rhythmical movements of the head synchronous with the pulse (Musset's sign), rhythmical change in the colour of the nail bed under a slight pressure on the nail end, the so-called capillary pulse (Quin-cke'sjpulse), rhythmical reddening of the skin after rubbing, etc.
The apex beat is almost always enlarged and shifted to the left and in-feriorly. Sometimes, along with the elevation of the apex beat, a slight depression in the neighbouring intercostal spaces can be observed. The apex beat is palpable in the sixth and sometimes seventh hypochondrium, anteriorly of the midclavicular line. The apex beat is diffuse, intense, and rising like a dome. This indicates significant enlargement of the left ventricle. The border of cardiac dullness can be found (by percussion) to shift to the left; the heart becomes " aortic" (with pronounced waist of the heart).
Auscultation reveals decreased first sound at the apex, since during left-ventricular systole the period when the valves are closed is absent. The second sound on the aorta is also weak, and if the valve is damaged significantly, it can be inaudible. The second sound can be quite loud in atherosclerotic affection of the aorta. Diastolic murmur heard over the aorta and at the Botkin-Erb listening point is characteristic. This is a low blowing protodiastolic murmur which weakens by the end of diastole as the blood pressure in the aorta drops and the blood-flow rate decreases. The described changes in the sounds and murmurs are clearly visible on
Special Part
Chapter 6. Blood Circulatory System
 |
| —^4—j|--------------------------- ^ — |
| Iff— —M^^k^*™.—^_--------- wmfm*M*---- vM*----- |W/v |

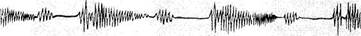
Fig. 75. 5CG in aortic incompetence. The amplitude of the heart sounds and diastolic murmur are decreased on the ECG taken over the aorta.
phonocardiograms (Fig. 75). Murmurs of functional aetiology can also be heard in aortic incompetence at the heart apex. If the left ventricle is markedly dilated, relative mitral incompetence develops and systolic murmur can be heard at the heart apex. Diastolic murmur (presystolic or Austin Flint murmur) can sometimes be heard. It arises due to an intense regurgitation of the blood that moves aside the mitral valve cusp to account for functional mitral stenosis. Doubled sound (Traube double sound) and doubled Vinogradov-Duroziez murmur can sometimes be heard over the femoral artery in this disease.
The pulse in aortic incompetence is fast, full, and high, which is due to high pulse pressure and increased volume of blood delivered into the aorta during systole. Arterial pressure constantly varies: the systolic pressure rises and diastolic falls, and the pulse pressure is therefore high.
X-ray studies show an enlarged left ventricle with a distinct waist of the heart (Fig. 76) and dilatation of the aorta; pulsation of the aorta is intense.
The ECG also reveals various signs of hypertrophy of the left ventricle (Fig. 77): the electrical axis is deviated to the left, the S waves in the right chest leads are deep and the amplitude of the R wave is higher in the left chest leads; these signs often combine with signs of overstrain in the left ventricle and relative coronary insufficiency (changes in the terminal part
of the ventricular complex, displacement of the S-T interval, and the negative T wave).
Echocardiograms taken from patients with aortic failure show flutter of the anterior mitral cusp during diastole caused by the thrust of the blood regurgitated from the aorta into the ventricle.
Aortic incompetence can for a long time be compensated for by intensified work of the hypertrophied left ventricle. When its contractile force decreases, congestion in the lesser circulation develops. Acute weakness of the left ventricle sometimes develops and is manifested by an attack of cardiac asthma. Dilatation of the weakened left ventricle can cause relative mitral incompetence. This increases venous congestion in the lesser circulation associated with decompensated aortic incompetence and adds to the load on the right ventricle. This is mitralization of aortic incompetence, which may become the cause of venous congestion in the greater circulation.

Fig. 76. X-ray in aortic incompetence. The heart's configuration is aortic; the left ventricle is dilated and hypertrophied, the ascending aorta is dilated.
Special Part
Chapter 6. Blood Circulatory System
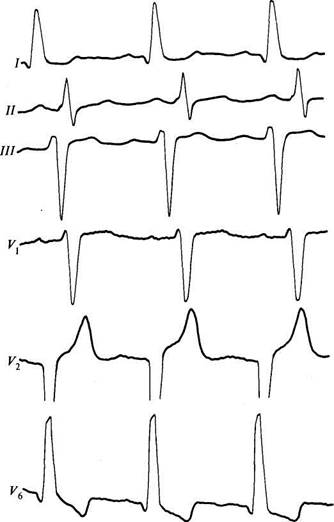
Fig. 77. ECG in aortic incompetence. AORTIC STENOSIS
The narrowing of the aortic orifice (aortic stenosis) interferes with expulsion of blood into the aorta during contraction of the left ventricle. Aortic stenosis is usually caused by rheumatic endocarditis; less frequently
ll
it develops due to bacterial endocarditis, atherosclerosis, or it may be congenital. Stenosis results from adhered aortic valve cusps or develops due to cicatricial narrowing of the aortic orifice.
Haemodynamics. During systole, the left ventricle is not emptied completely because part of blood fails to pass the narrowed orifice into the aorta. A new normal portion of blood delivered during diastole from the left atrium is mixed with the residual volume and the ventricle becomes overfilled. The pressure inside it thus rises. This disorder is compensated for by an intensified activity of the left ventricle to cause its hypertrophy (Fig. 78).
Clinical picture. Aortic stenosis can remain compensated for years and would not cause any unpleasant subjective sensations (even during intense physical exertion). If obstruction of the aortic orifice is considerable, insufficient blood ejection into the arterial system upsets normal blood supply to the hypertrophied myocardium and the patient feels pain in the heart (angina pectoris-type pain). Disordered blood supply to the brain is manifested by giddiness, headache, and tendency to fainting. These symptoms like pain in the heart would more likely occur during physical exercise and emotional stress.
The skin of the patient is pallid due to insufficient blood supply to the arterial system. The apex beat is displaced to the left, less frequently in-feriorly; it is diffuse, high, and resistant. Systolic thrill (cat's purr) can be palpated in the region of the heart. Percussion reveals displacement of the left border; the heart is " aortic" due to hypertrophy of the left ventricle. Auscultation of the heart at its apex reveals diminished first sound due to overfilling of the left ventricle and prolongation of systole. The second sound is diminished over the aorta. If the aortic cusps adhere and are im-
| Fig. 78. Upset intracardiac haemodynamics in stenosed aortic orifice (for designations see Fig. 69). |
| 20-1556 |
 L/C
L/C
(Special Part
Chapter 6. Blood Circulatory System
 |
|
| (1 m ft m |
Fig. 79. PCG and sphygmogram in aortic stenosis. The PCG taken over the aorta shows crescendo-decrescendo (diamond-shaped) systolic murmur; the peak of the sphygmogram is
serrated like a cock's comb.
mobile, the second sound can be inaudible. Rough systolic murmur over the aorta is characteristic. This murmur is generated by the blood flow through the narrowed orifice. It is conducted by the blood onto the carotids and can sometimes be heard in the interscapular space. The pulse is small, slow, and rare, since the blood slowly passes into the aorta and its volume is decreased. Systolic arterial pressure is usually diminished, while diastolic remains normal or increases. The pulse pressure is therefore decreased.
X-ray examination shows hypertrophied left ventricle, " aortic" configuration of the heart, and dilatation of the ascending aorta (post-stenotic); the cusps of the aortic valve are often calcified.
The ECG usually shows signs of hypertrophy of the left ventricle and sometimes of coronary insufficiency. The phonocardiogram shows the specific changes in the heart sounds: diminished amplitudes of the first sound at the heart apex and of the second sound over the aorta. Systolic murmur over the aorta is typical; its oscillations are recorded in the form of specific diamond-shaped figures (Fig. 79).
Sphygmograms of the carotids reveal slowed ascent and descent of the pulse wave (slow pulse), small amplitude of the pulse waves, and specific serrated pattern of their peaks (sphygmograms in the form of a cock's comb) showing oscillations associated with conduction of systolic murmur onto the neck vessels.
Echocardiograms show decreased opening of the aortic valve during systole. Echoes from the cusps become more intense and signs of hypertrophy of the left ventricle appear.
Aortic stenosis remains compensated for a long time. Circulatory insufficiency develops in diminished contractility of the left ventricle and it is manifested as in aortic incompetence.
TRICUSPID INCOMPETENCE
Insufficiency of the tricuspid valve can be functional (relative) and organic (permanent). Organic tricuspid incompetence occurs in rare cases, mainly due to rheumatic endocarditis. Tricuspid incompetence usually combines with affections of other heart valves; as an independent disease, it occurs in exceptionally rare cases.
Relative (functional) insufficiency of the tricuspid valve occurs more often. It is due to dilatation of the right ventricle and distention of the right-atrioventricular orifice. Tricuspid incompetence often combines with mitral diseases because the right ventricle has to perform greater work due to the high pressure in the lesser circulation. This causes overstrain and distention of the right ventricle.
Haemodynamics. Due to incomplete closure of the tricuspid valve during right-ventricular systole, part of blood is regurgitated into the right atrium, where it is mixed with the normal volume of blood delivered from the venae cavae. The atrium thus becomes distended and hypertrophied. During diastole, a larger volume of blood is delivered into the right ventricle from the right atrium because the portion of blood that was regurgitated into the atrium during systole is added to the normal volume of blood delivered. This causes dilatation and hypertrophy of the right ventricle (Fig. 80). Compensation in this disease is attained by intensified work of the right atrium and the right ventricle whose compensatory power is not great and congestion in the greater circulation therefore soon develops.
Clinical picture. Pronounced venous congestion in the greater circulation in the presence of tricuspid incompetence causes oedema, ascites, feeling of heaviness and right hypochondriac pain (due to enlargement of the liver). The skin becomes cyanotic, sometimes with a yellowish tint. The neck veins swell and pulsate; the positive venous pulse and pulsation of the liver are also observed. These pulsations are explained by the regurgitation
|
|