
Главная страница Случайная страница
Разделы сайта
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Laboratory and Instrumental Methods of Examination
|
|
Laboratory and instrumental methods of examination are quite varied and their number constantly increases. As distinct from the main methods, such as inquiry, inspection, palpation, percussion and auscultation, the instrumental and laboratory methods depend on the advances in modern physics, chemistry, biology and related sciences; these methods require more sophisticated instruments and equipment (thermometers, electrocardiographs, X-ray units, laboratory equipment, etc.) and a specially trained
medical personnel (laboratory technicians, physicians, roentgenologists and others).
Wide use of laboratory and instrumental techniques in the clinical and experimental practice for examination of patients facilitates the study of the disease, helps discover new, earlier unknown diseases and, what is more important, it ensures earlier diagnosis of the disease and hence its timely treatment. The laboratory and instrumental methods were formerly known as additional techniques since they are used not in all cases and only after examination of the patient by the main diagnostic methods. But they are now widely used in medicine and sometimes the results of instrumental and laboratory examination become so important that the physician cannot establish a correct diagnosis without using them first. This section describes only general principles of the laboratory and instrumental methods of examination. They will be given in more detail during discussion of diseases of separate organs and systems.
Anthropometry
Anthropometry (Gk anthropos human being and metron measure) is the method of examination based on the comparative measurements of morphological and functional signs of man. Measurement of comparatively small number of signs is sufficient for practical medicine (clinical anthropometry). The main anthropometric sings are the man's height and
weight.
The man's height depends on the dimensions of the skeleton and is determined by the height meter. The normal height of males varies from 165 to 180 cm and of females from 155 to 170 cm. Deviations on either side are connected with endocrine dysfunction. Dwarf ism may be due to hypofunction of the anterior lobe of the pituitary (nanism) or of the thyroid gland (cretinism). Gigantism can be due to dysfunction of the anterior lobe of the pituitary or hypofunction of the sex glands.
The height of man is measured by a wooden or metal graduated plank fixed in a floor-mounted base. A horizontal plank slides freely along the vertical plank to read the height. A special collapsible seat is provided to measure the sitting height (the length of the trunk). Another graduated scale begins reading at the level of the seat. In order to measure the height of a man, he is asked to stand barefoot on the floor plate and to assume an erect attitude so that his back is pressed against the vertical plank; the head should be in a position where the upper edge of the external auditory meatus is level with the outer angle of the eye. The sliding horizontal plank is then lowered to come in contact with the patient's head and fixed in this Position. The patient is asked to step out from the height meter. The lower edge of the sliding Plank reads the height. The sitting height is measured in the same way except that the patient is asked to sit.
. Patient's height and the length of his trunk are important for the assess-ment of both his physical growth and proportions of his separate parts
General Part
Chapter 3. Methods of Clinical Examination
which can be upset in some congenital diseases (e.g. chondrodystrophy) and diseases acquired in childhood.
In addition to measurement of the patient's height (and sitting height), measured also are the girth of his chest, abdomen, neck, head, lower extremities, pelvis, and some internal organs (by percussion). The technique and importance of measurements will be discussed in relevant chapters.
Weight is measured on a special medical balance. Weighing should be done in the morning, on a fasting stomach, after defaecation and urination. Whenever possible, the patient should be with no clothing or he should wear a light garment. In order to follow changes in the patient's weight during treatment (e.g. in treatment of asthenia or obesity, treatment of oedema, etc.) repeated weighings should be done in the same conditions (with the patient either undressed or with the same clothes on) in order to rule out the error.
The weight of the human body depends mainly on the height and the girth of the chest. The correlation between these two factors determines proportionate constitution of man. Normal weight can be calculated approximately by measuring the man's height and subtracting 100. For example the normal weight of a 180 cm high man should be 80 kg (180 - 100).
The following factors are practically important:
1. The statural-weight value. It reflects proportionality of height to weight and is determined by the formula
Px 100
 where P is the weight of the body in kg and a is the height in cm. The normal height to weight ratio is expressed by the index 37- 40. Lower index indicates malnutrition and higher overfeeding of the patient.
where P is the weight of the body in kg and a is the height in cm. The normal height to weight ratio is expressed by the index 37- 40. Lower index indicates malnutrition and higher overfeeding of the patient.
2. The index of proportionality between height (a) and the girth of the
chest (T) is determined by the formula
Tx 100
 a
a
Normal index is from 50 to 55; lower figures indicate narrow chest (stenothorax), and higher broad chest.
3. The normal proportional ratio between the three parameters a -
- (T + P) is about 20 and it deviates significantly if this proportion is ab
normal.
Muscular force is measured by dynamometry. The patient is asked to compress an elliptic steel spring provided with a scale and a reading arrow. Other devices are also available by which power of various muscles can be measured.
Thermometry
Body temperature is measured in each patient. It helps reveal fever and is very important diagnostically. Fever is usually caused by infection and products of tissue decomposition. Fever is a normal reaction of the body to infection. Sometimes an infectious disease can develop without fever or it can temporarily proceed without elevation of temperature (tuberculosis, syphilis). The degree to which the body temperature rises depends on the patient's condition: the same infection can cause different fever in various persons. For example, in the young the temperature in pneumonia rises to 40 °C and over, while in old or asthenic patients with the same disease the temperature rises insignificantly or it may remain at normal level.
Elevation of temperature unconnected with infection is sometimes observed in malignant tumours or tissues necrosis (e.g. in myocardial infarction), tissue haemorrhages, rapid decomposition of red blood cells in the blood, etc. Fever occurs less frequently in diseases of the central nervous system and also in diseases of reflex aetiology. Non-infectious fever does not strongly affect the patient's condition and is usually transient.
The temperature is measured by a thermometer graded in 0.1 ° (C or F). Electric thermometers are also used in medical research. The sensitive element in such thermometers is a thermocouple. An electric thermometer quickly responds to variations in temperature. It can be used to measure and compare temperature of various areas of the skin. Some electric thermometers (including multi-channel) are provided with a device that automatically records variations in temperature on a graph paper (elec-trothermographs).
When temperature is measured, the thermometer is kept in the armpit for about ten minutes. The thermometer should come in tight contact with the patient's skin; the forearm should be tightly pressed against the chest to close the armpit. When temperature is measured in asthenic patients or in children, assistance is required to keep their forearm pressed to the chest. Sometimes temperature is measured in the rectum for which purpose the thermometer coated with oil is inserted in the rectum; the patient should lie on his side. Rectal temperature is 0.5- 1° higher than in the armpit.
As a rule temperature is taken twice a day (at 7 or 8 a.m. and 5 or 7 P-m.). Thermometer readings should be registered on a special chart for several days where the morning and the evening temperature is designated by dots. The dots are then interconnected to give a curve which is characteristic for many specific diseases.
Normal temperature of the body (as measured in the armpit) is 6-4-36.8 °C. The temperature undergoes circadian variations. The °west temperature is between 3 and 6 a.m. and the maximum between 5 nd 9 p.m. The difference between the morning and evening temperature
64.
General Part
Chapter 3. Methods of Clinical Examination
does not exceed 0.6 °C in normal persons. The temperature of the body slightly rises after meals and physical strain, and also at high ambient temperatures.
Fever is characterized not only by elevated temperature but also by the upset function of the entire body. The rise in temperature is a very important (but not always decisive) sign for assessing severity of fever. It is accompanied by accelerated pulse and respiration rate; arterial pressure often drops; the patient complains of being hot, exhausted, of headache, dry-ness and the unpleasant feeling in the mouth, thirst, and the absence of appetite; the tongue is coated and often dry; the amount of excreted urine decreases. Fever intensifies metabolic processes. And since the patient would often refuse food, his weight often decreases significantly.
A quick and intense rise in temperature (e.g. in malaria or pheumonia) is often attended by chills, which can last from a few minutes to an hour, and in rare cases for longer periods. The skin blood vessels strongly contract in chills, the skin becomes pallid, goose-flesh (cutis anserina) appears, the nailbeds become cyanotic; the patient feels intense cold, he shivers, the teeth begin chattering. If the temperature rises gradually, the chills are only slight. At high temperature the skin reddens and becomes warm; the patient feels hot. A sudden drop in temperature is accompanied by heavy perspiration. The temperature of the patient with fever is higher in the evening than in the morning. Its rise over 37 °C suggests a disease.
Elevated temperatures are characterized as follows (Fig. 6): temperatures from 37° to 38 °C are called subfebrile, from 38° to 39 °C moderately high, from 39° to 40 °C high, and over 40 °C very high. Temperatures over 41° and 42 °C are called hyperpyretic and are dangerous to the patient's life.
Not only elevated temperature itself but also its circadian variations are very important for diagnosing the diseases. Variations of temperature during the day determine the type of fever (Fig. 7). The following main six types of fever are differentiated.
1. Continued fever {febris continua). The circadian variation does not
exceed 1 °C. It is observed in patients with acute lobar pheumonia or II
stage typhoid fever.
2. Remittent fever {febris remittens). The circadian variations exceed
1 °C, the morning lowest temperature being over 37 °C; it often occurs in
tuberculosis, III stage typhoid fever, purulent diseases, and lobular
pneumonia.
3. Intermittent fever {febris intermittens). The daily variations exceed
1 °C, with complete apyrexia in remissions.
4. Hectic fever (febris hectica). The temperature rises sharply (by
2°-4 °C) and drops to normal and subnormal level. The fever is often ac-
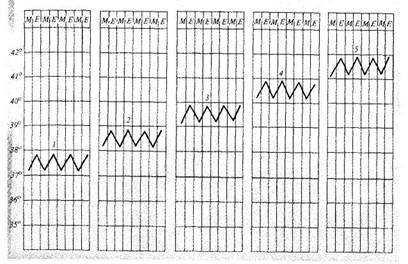
Fig. 6. Types of fever.
1— subfebrile (37-38 °C); 2— moderate (38-39 °C); 3— high (39-40 °C); 4— very high (over 40 °C);
5 —hyperpyretic (over 41-42 °C).
companied by excessive sweating. It usually occurs in grave pulmonary tuberculosis, suppuration, and sepsis.
5. Inverse fever {typhus inversus). The morning temperature is higher
than in the evening; it sometimes occurs is sepsis, tuberculosis, and
brucellosis.
6. Irregular fever {febris irregularis). Circadian variations are varied
and irregular. It often occurs in rheumatism, endocarditis, sepsis, tuber
culosis, etc.
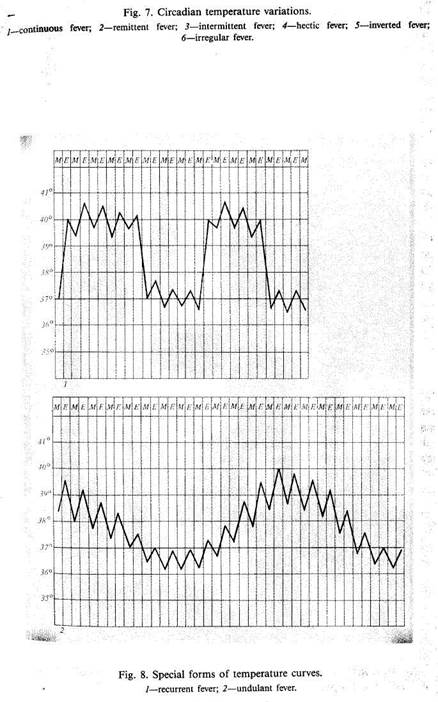
According to the temperature curve (Fig. 8) recurrent (relapsing) and undulant (Malta) fevers are distinguished.
Recurrent fever {febris recurrens) is characterized by alternation of lever and afebrile periods; it occurs in relapsing fever.
Undulant fever (febris undulans) is characterized by periodic elevation ot temperature followed by its drop; it often occurs in brucellosis and lym-Phogranulomatosis.
^ The course of fever (Fig. 9) is characterized by aperiod of elevation of ^rnperature (stadium incrementi), which is followed by the period of high ^" ^ ^asti^ium^' and ending with the period of decreasing erature (stadium decrementi). The temperature may decrease gradually,
5-1556
|

|
General Part
Chapter 3. Methods of Clinical Examination
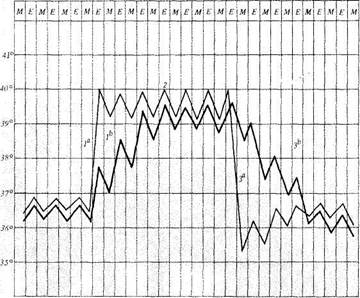
Fig. 9. Periods of temperature curves. /", /*—two variants of stadium incrementi; 2 —stadium fastigii; 3", 3b —two variants of stadium decrement.
during several days. This termination of fever is called lysis. A sudden temperature drop (to norm within 24 hours) is called crisis. During abatement of fever in some diseases (e.g. in typhoid fever), the daily variation of temperature exceeds 1 °C {amphibolic period).
Regular alternation of fever attacks (chills, heat, temperature drop with
sweating) and afebrile periods is characteristic of malaria. Attacks may oc
cur every day (febris quotidiana), every other day {tertian fever, or febris
tertiana) or every third day {quartan fever, or febris quartana). The
temperature rise may be only transient, for few hours (one-day fever, or
febris ephemera, febriculara.) It occurs in mild infection, excess exposure
to the sun, after blood transfusion, sometimes after intravenous injections
of medicinal preparations.
Fever lasting up to 15 days is called acute, and over 45 days—chronic.
Hypothermia (subnormal temperature) often occurs in the critical fall of temperature; it persists for 1-2 days at about 35 °C; the pulse is full, slow, the patient's condition satisfactory. Subnormal temperature may be observed in grave circulatory collapse; the pulse becomes weak and frequent, respiration superficial, the skin pallid and covered with sweat. Hypothermia occurs after profuse bleeding, in starvation and asthenia, during convalescence after infectious diseases, and in overcooling.
In addition to measuring the body temperature with a thermometer, the temperature of various parts of the body should be felt by hand. Elevated temperature of the skin overlying a joint indicates its inflammation; cold extremities of patients with fever suggest peripheral circulatory failure (collapse, cardiac insufficiency).
Since 1970, thermography—thermovision—has been introduced in practical medicine in the Soviet Union. The method is based on detection of zones with increased infra-red radiation emanating from the organs affected by acute inflammatory, cancerous, and other diseases by using special apparatus—thermovision system.
Measuring temperature inside some hollow organs (stomach, large intestine, etc.) by special radio devices is of great diagnostic significance.
X-Ray Study
Roentgenoscopy, or examination with X-rays by means of a fluorescent screen, is widely used in therapeutic practice. But routine non-contrast roentgenoscopy makes it possible to examine only organs that produce shadows of different intensity on a screen. For example, the heart can be examined (its dimensions and shapes) against the background of lungs which are transparent on an X-ray screen. Consolidated parts of pulmonary tissue (inflammatory infiltration in pneumonia, tumour, etc.) can also be seen on an X-ray screen.
When it is necessary to record some changes radiography (the making of X-ray pictures) is resorted to. It should be kept in mind that the pattern obtained on an X-ray film is negative, i.e. the parts that are light on an X-ray screen appear as black on the film and vice versa.
In order to examine hollow organs (stomach, intestine, gall bladder, renal pelves, etc.) which produce on a screen a dense uniform shadow, a special contrast substance should first be given to the patient. Barium sulphate is given before examining the gastro-intestinal tract; when the large intestine is examined the suspension of barium sulphate is administered as an enema. Iodine preparations are given to examine the gall ladder and intrahepatic bile ducts {cholecystography, cholegraphy). Some
does not exceed 0.6 °C in normal persons. The temperature of the body slightly
General Part
preparations (e.g. bilitrast or iopanoic acid) are given per os while others (e.g. bilignost) intravenously. These substances are carried by the blood to the liver and excreted together with bile to accumulate in the gall bladder. X-ray examination of the renal pelves (pyelography) is done with sergosin given intravenously as well. In X-ray examination of the bronchi ipron-chography) they are filled with a special contrast substance (iodolipol); car-diotrast is used in angiography (X-ray examination of the blood vessels). Sometimes an X-ray image of an organ becomes more distinct after the surrounding tissues or cavity are filled with air. During X-ray examination of the kidneys for suspected tumour, air is injected into the perirenal fat; the abdominal cavity is filled with air to reveal growth of the tumour into the stomach walls (artificial pneutnoperitoneum).
A number of new improved X-ray techniques have been elaborated recently. For example, roentgenokymography is used to examine the moving organs such as the heart. A special lead plate is interposed in the path of X-ray emitted by the X-ray tube and passed through the examined part. The plate has horizontal slits and moves through a certain distance in the plane perpendicular to the contour of the examined organ. Since the organ (e.g. the heart) moves, the X-ray image on the film is in the form of a toothed line. The amplitude and the shape of the teeth are informative of the contractile strength of the heart and the character of its contractions. Tomography or sectional radiography is often used as well. During an exposure, the X-ray tube is moved so that the selected structures only remain stationary on the moving film and their image is clear and sharp while structures located at other depths (in all other planes) have a relative displacement on the film and appear obliterated or blurred. Tomography is used to reveal tumours, inflammatory infiltrations and other pathological growths. Computer tomography has become popular in recent times.
The quality of images has improved significantly during the past years. X-ray machines are now equipped with special electronic optical amplifiers which give brighter and more distinct images, while the time of a patient's exposure to X-rays is diminished. This makes it possible to film the entire process of examination or its separate stages (cineradiography). It is especially important in functional disorders of organs (oesophagospasm, dyskinesia of the intestine, etc.). The film can be reviewed as many times as may be necessary, which is important at consultation, etc. The electronic optical devices can transmit the image to TV receivers, whose screens give a more distinct picture than an ordinary X-ray machine. The screen of a special TV set can be demonstrated remotely in places protected from excess radiation. All manipulations with the X-ray machine (its adjustment in the vertical or horizontal plane, taking pictures, etc.) can be done at a distance from a remote control panel.
Chapter 3. Methods of Clinical Examination 71
Endoscopy, Biopsy, and Cytological Studies
Endoscopy (Gk endon within, skopein to watch) is the examination of the interior of hollow or tubular organs by direct observation of their internal surface by means of endoscopes. The simplest endoscope is a metal tube (or two collapsible tubes) provided with an optical system that enlarges the image, and an illuminating device. New types of endoscopes have been devised recently. The image is transmitted in them through fibrous light guides (optical fibres). The main advantage of these endoscopes is their high flexibility which facilitates examination and makes it practically safe.
Endoscopy is used for inspecting the oesophagus (pesophagoscopy), stomach (gastroscopy), duodenum (duodenoscopy), rectum and sigmoid colon (rectoromanoscopy), the entire large intestine (colonoscopy), trachea and bronchi (tracheobronchoscopy), the abdominal cavity and its organs (laparoscopy), urinary bladder icystoscopy), and of some other organs. A special endoscope is used in each particular case, the design of the instrument being specially adapted to the anatomophysiological properties of the particular organ.
The diagnostic value of endoscopy increases because specimens of mucosa or tissues of the examined organ can be taken (biopsy). These samples are used for cytological, histological, and histochemical analyses. Biopsy can however be an independent procedure (without endoscopy). " Blind" biopsy is used to take specimen of mucosa of the stomach or duodenum, of the liver tissue (transcutaneous biopsy) and kidneys; sternal puncture is used for taking samples of bone marrow, etc. Photographic pictures can be taken during endoscopy using special photographic adaptors. Modern endoscopes can transmit the picture onto a TV screen so that other physicians engaged in the treatment of a given patient can also observe the changes revealed by endoscopy. Video tape-recorder makes it possible, whenever necessary, to compare the picture with the results of repeated endoscopy (e.g. to follow cicatricial changes in gastric ulcer, etc.).
Endoscopy is oft.en used for therapeutic purposes as well. Foreign bodies and polyps can be removed by an endoscope, ulcers can be cauterized, and other manipulations can be performed under control of an endoscope. It should be remembered that endoscopy can only be carried out by a specially trained physician and for special indications because complications can arise due to anaesthesia and narcosis (which are often used to make endoscopy painless) and to endoscopy itself. Ophthalmoscopy (inspection of the fundus of the eye) and capillaroscopy (examination of the capillaries in the nailbed) resemble endoscopy in certain respects for both re used for diagnosis of internal pathology (essential hypertension, aiabetes mellitus, etc.).
General Part
Chapter 3. Methods of Clinical Examination
Instrumental-Functional Methods of Examination Various methods are used in the clinic to study functional activity of various organs. These methods can conventionally be divided into three groups. The first group includes methods based on the recording of biopotentials arising during functioning of the organs. These are elec-trocardiography, electroencephalography, electrogastrography, and elec-tromyography. The second group includes methods by which motor activity (kinetics) of organs is recorded. These are " bulb" kymography of various parts of the gastro-intestinal tract (done with a rubber tube ending with a rubber bulb; the other end of the tube is communicated with an instrument which records all variations in pressure inside the air-filled bulb resulting from contractions of the oesophagus, stomach, or the intestine); study of peristalsis and pressure inside the alimentary organs by means of a radio-capsule; apical cardiography (recording the apex beat)! oesophagoatriography (recording of pressure variations inside tb oesophagus which are transmitted from the adjoining left atrium) ballistocardiography (recording vibrations of the human body caused by heart contractions and the reactive forces); rheography (registration of? changes in the tissue resistance in connection with the circulatory dynamics during heart contractions); spirography and pneumotachymetry (registration of the outer respiration function). The third group includes the] methods by which various sounds generated during contraction and move-1 ment of various organs are recorded. The most important of them is phonocardiography (recording heart sounds). Phonopneumography and 9 phonointestinography (recording sounds arising in the lungs and the in- || testine) are less popular.
Radioisotope Methods
Radioisotope methods of study are now coming into wide use. Scanning is among them. The patient is given a radioactive preparation that can concentrate in the desired organ: 131I and 132I are used to examine the thyroid; iodine-labelled rose bengal or a colloidal solution of gold (198Au) are used to study the liver; neohydrin labelled with mercury isotopes 197Hg or 203Hg are given to study the liver, etc. The patient is placed on a bed beneath a detector of the scanning apparatus (gamma-topograph or a scanner). The detector (scintillation counter of gamma-radiation) moves along a predetermined line over the object of study and receives the radioactive impulses emitted from the examined organ. Signals of the counter are modified by a collimator into various forms of records (scin-
tiscans or scans). The results of scanning can be recorded either graphically as a black-and-white or colour shaded pictures, photographically, or digitally (after processing of the information on a computer). Since the radiation intensity over the organ where the radioisotope is accumulated is much higher than over the surrounding tissues or organs, the density of lines or points are higher on the portion of the scan corresponding to this organ. Thus a " shadow" picture of the organ under examination is obtained on a scan. In focal affections of the parenchyma of an organ (tumour, cyst, abscess, etc.) rarefied foci can be distinguished on the scan.
Scanning can be used to determine displacement of the organ and changes in its size and functional activity (by diffuse lessening of density on the scan). It is used to study the thyroid, liver, kidneys and (less frequently) some other organs.
Radioisotopes are widely used to study the function of some organs. The rate of entrance and accumulation of a radioactive isotope in a given organ, and also removal of the isotope from the body are studied. The function of the thyroid gland is assessed by the dynamics of the absorption of sodium iodide (131I) in the thyroid, and concentration of protein-bound 131I in the patient's blood plasma. Renal function is studied by the rate of discharge of 131I-labelled hippuran. Radioactive isotopes are used to study absorption in the small intestine and also for some other investigation.
Ultrasound Echography
Ultrasound echography (syn. echolocation, ultrasound scanning, sonography) is a diagnostic method based on different reflection of ultrasound waves that pass at various velocities through tissues and media of various density. Ultrasound is acoustic frequency from 2 X 104 to 108 Hz, which are not perceived by the human ear. Ultrasound well propagates in body tissues even at low energies (0.005-0.008 W/cm2), which is hundreds or thousands times lower than the doses used for therapeutic purposes (ultrasound therapy). Ultrasound travels in the human body at a velocity of about 1 500 m/s. Using ultrasound for diagnostic purposes is based on its ability to propagate in media in a given direction in the form of a fine concentrated beam of waves. Ultrasound waves are differently absorbed (damped) in various tissues and differently reflected from them. Sensitive instruments differentiate reflection of ultrasound pulses from tissues if weir density differs as slightly as by only 1 per cent. This makes ultrasound a useful diagnostic aid. Modern apparatus produce ultrasound pulses lasting for 2-5 jts at a frequency of 1000 Hz at short intervals of time. The
General Part
Chapter 3. Methods of Clinical Examination
reflected ultrasound pulses are detected, transformed, and transmitted to an oscilloscope from which the pulses are read off.
First attempts to use ultrasound for diagnostic purposes were undertaken more than 35 years ago, but satisfactory technical apparatuses have been devised and introduced into clinical practice only during recent time.
The advantage of ultrasound is that it can be used to determine the structure of various organs without producing any harmful effect on the patient; moreover the procedure is not in the least annoying to the patient. The examination can be repeated (for example in order to assess the dynamics of the process) without any detriment to the patient. Great diagnostic reliability and the value of data obtained with ultrasound make this method very important. It has advantages in comparison with other methods since it needs no contrast, radioactive, or other substances to be given to the patient before the procedure.
Ultrasound is obtained by conversion of energy of electromagnetic oscillations (the inner piezoelectric effect). The phenomenon is based on the property of some crystals to change their electric charge under the compressing or stretching effect. The value of the charge is directly proportional to the mechanical pressure applied. This phenomenon is used in ultrasound diagnostic apparatus for recording the sound oscillations. The reverse piezoelectric effect, by which electric energy is converted into acoustic energy, is utilized for the generation of ultrasound energy.
Transmission and location (echography) ultrasound methods are used for examination of patients. The transmission method is seldom used. The source of ultrasound oscillations is applied to one side of the patient while the receiver of the ultrasound beam is positioned on the other side. The location method is however more popular. The piezocrystal is used as both the source of ultrasound and as the receiver. Ultrasound is converted into electric energy and the structure of the studied organ can be visualized on the screen of an oscilloscope.
One- and two-dimensional methods of visualization are used. In the one-dimensional (A-method) echography, ultrasonic waves reflected from the studied object are converted into electric pulses and delivered onto the vertically deviating plates of an X-ray tube. Whenever several anatomical media, located at different distances from the receiver, arise in the pathway of the ultrasonic beam, the vertical spikes are fixed on the horizontal scanning in succession, in accordance with the time of arrival of the ultrasonic pulse reflected from this or that object. Since this process is repeated at high frequency, the scanning line with spikes on it appears as a stationary pattern on the oscilloscope screen.
The A-method can be used to measure accurately the distance to the object under examination, to determine its anteroposterior dimensions, and sometimes to obtain information concerning special properties of the structure. The method fails to give complete information on the configuration and the size of the object studied, especially so if the object has irregular form.
The two-dimensional method (B-method) gives information about shapes, dimensions, and the structure of the object under study. The information is recorded on a Polaroid film, on a videotape, or common photographic film. Modern instruments give direct information
during the examination, which accelerates processing and interpretation of the data.
Systems with sectoral scanning are now also widely used. Electronic amplifiers and con-
verters of the echo-signals make it possible to record on the echogram 8—10 shades of grey
colour: from black to white.
Soviet-made apparatus " Echo-11" and " Echo-12" are widely used in echographic examinations though more improved models are being developed. The image is recorded from the oscilloscope of the echograph on a photographic film with the help of a camera.
Ultrasound is now widely used in the diagnosis of internal diseases, such as the diseases of the heart, liver, gall bladder, pancreas, kidneys, the thyroid, etc. The use of echography in cardiology makes it possible to determine the presence and character of heart defects, calcification of the cusps in rheumatism, tumour of the heart, and other changes in this organ. Ultrasonic echography is used in neurology (for the study of the brain, cerebral ventricles), in ophthalmology (to determine the optic axis of the eye, the degree of retinal detachment, to locate and assess the size of foreign bodies, to diagnose tumours of the eye and the orbit, etc.), in otorhinolaryngology (for differential diagnosis of loss of hearing), in obstetrics and gynaecology (to determine terms of pregnancy, multifoeta-tion, extrauterine pregnancy, to diagnose new growths of the female genitalia, pyo- and hydrosalpinx, to study the mammary glands, etc.), and in urology (to study the bladder, the prostate, etc.).
The Doppler effect is used for determining moving objects. Sound or light waves are reflected from the moving objects and return to their source with the changed wave frequency. This change is recorded by a receiving element and converted into an audible signal. Instruments utilizing the Doppler effect as their operating principle work with a continuous single frequency.
The ultrasonic Doppler system is used for assessment of the blood circulation parameters. The formed elements of blood (and other moving objects) reflect ultrasonic waves whose frequency is modulated. The modulation frequency is proportional to the velocity of motion of the studied object. Velocity is calculated as the difference between the emitted and received frequencies (Doppler formula). The Soviet-made echocardiograph (ultrasonic Doppler heart locator) is used for the study of kinetics of the heart valves and muscles and to measure the time of movements of the left and right chambers of the heart, which is especially important for the assessment of the myocardial function.
This brief analysis of the methods shows the importance of echography. In the opinion of experts, ultrasound will soon be used on a greater scale than X rays. According to some authors, a revolution is ex-Pected in medical diagnosis in the nearest future, because a branch of
medicine can hardly be found where ultrasound could not be used successfully.
General Part
Laboratory Methods of Examination
Laboratory methods are widely used in clinical practice. Excretions and secretions, excrements, the blood, exudates and transudates are analysed in the laboratory.
The laboratory investigations can be grossly classified as follows: (1) the study of the general properties of the examined material, the physical properties included (quantity, colour, appearance, odour, the presence of impurities, density, etc.); (2) microscopic studies; (3) chemical studies for the determination of the presence of certain substances (substances that are normally contained in various bodily fluids and excrements such as metabolites, microelements, hormones and products of their conversion, and substances appearing in disease); (4) bacteriological, proctological and virological studies; (5) serological diagnosis.
Chapter 4
|
|